© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
Private Health Insurance Quarterly Bulletin 85
(1 October–31 December 2017)
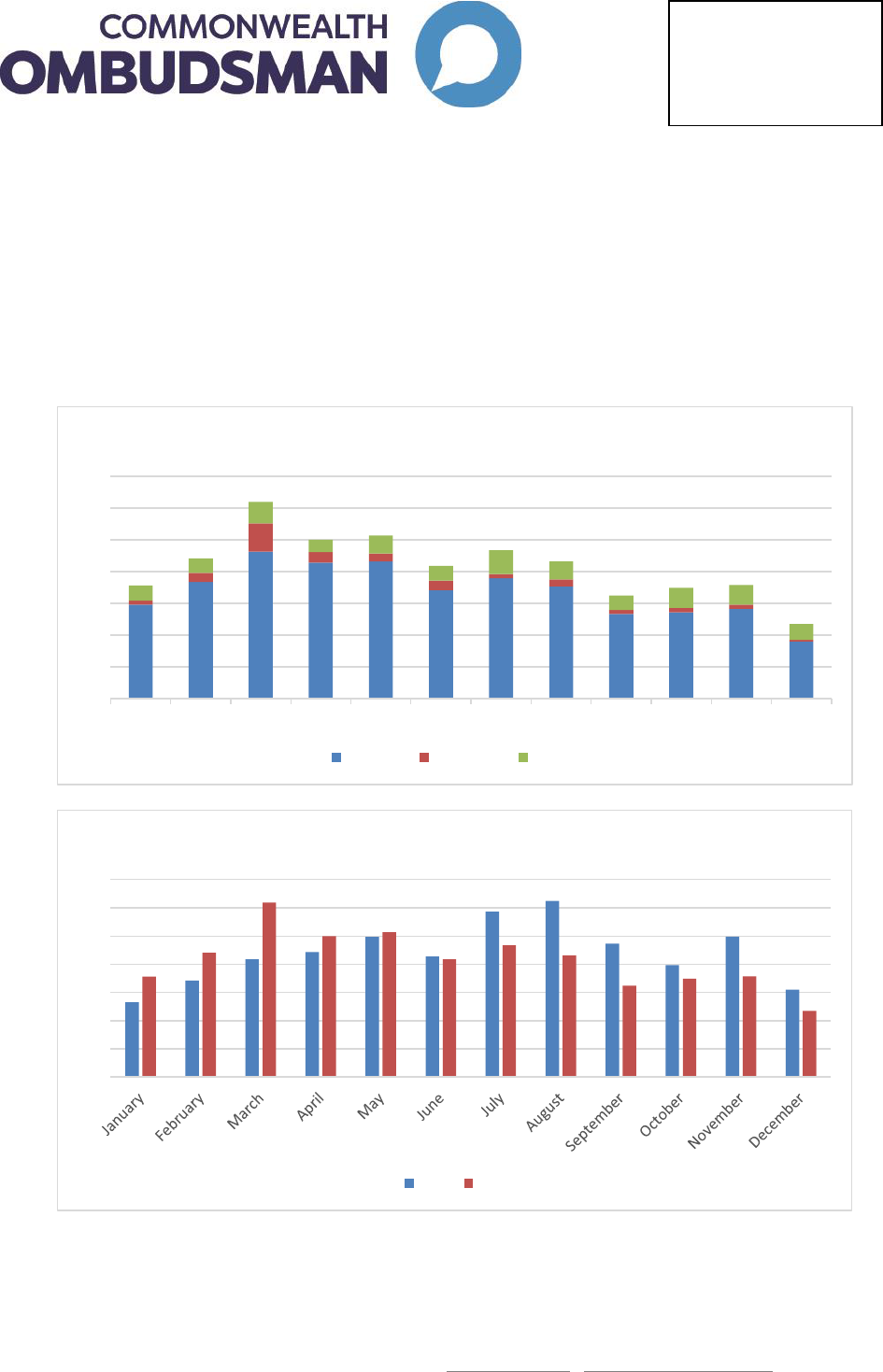
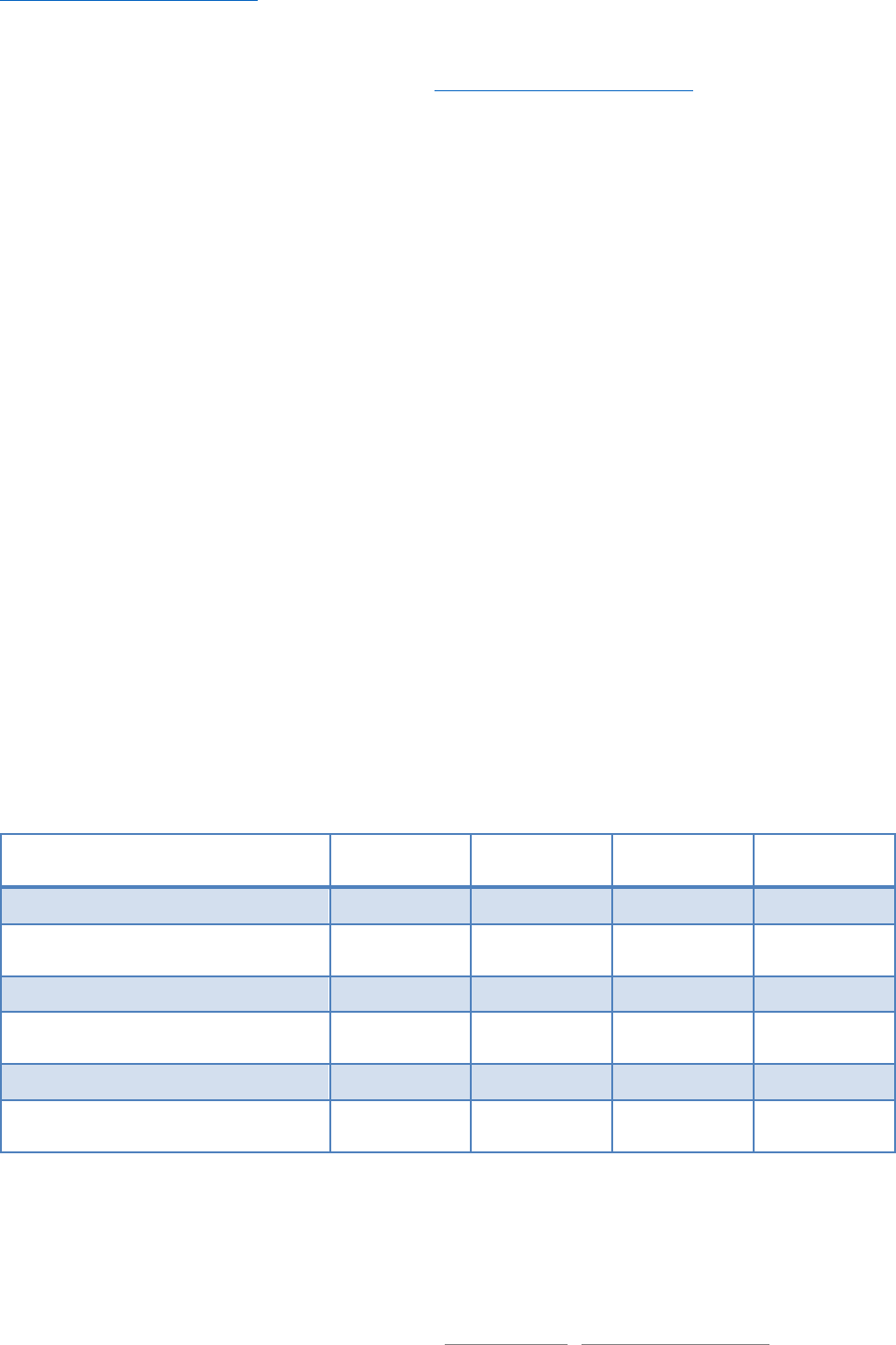
Complaint statistics this quarter
The Office of the Commonwealth Ombudsman (the Office) is pleased to report that private health insurance
complaints have returned to more average levels after a busy few quarters since mid-2016. Our Office
received 940 private health insurance complaints in this quarter. We received 1,204 complaints in the same
quarter last year, which represents a decline of 22 per cent from 2016 to 2017. In the previous quarter
ending September 2017, our Office received 1,222 complaints—representing a decline of 23 per cent.
0
100
200
300
400
500
600
700
Jan 17 Feb 17 Mar 17 Apr 17 May 17 Jun 17 Jul 17 Aug 17 Sep 17 Oct 17 Nov 17 Dec 17
Complaints by month
Problem Grievance Dispute
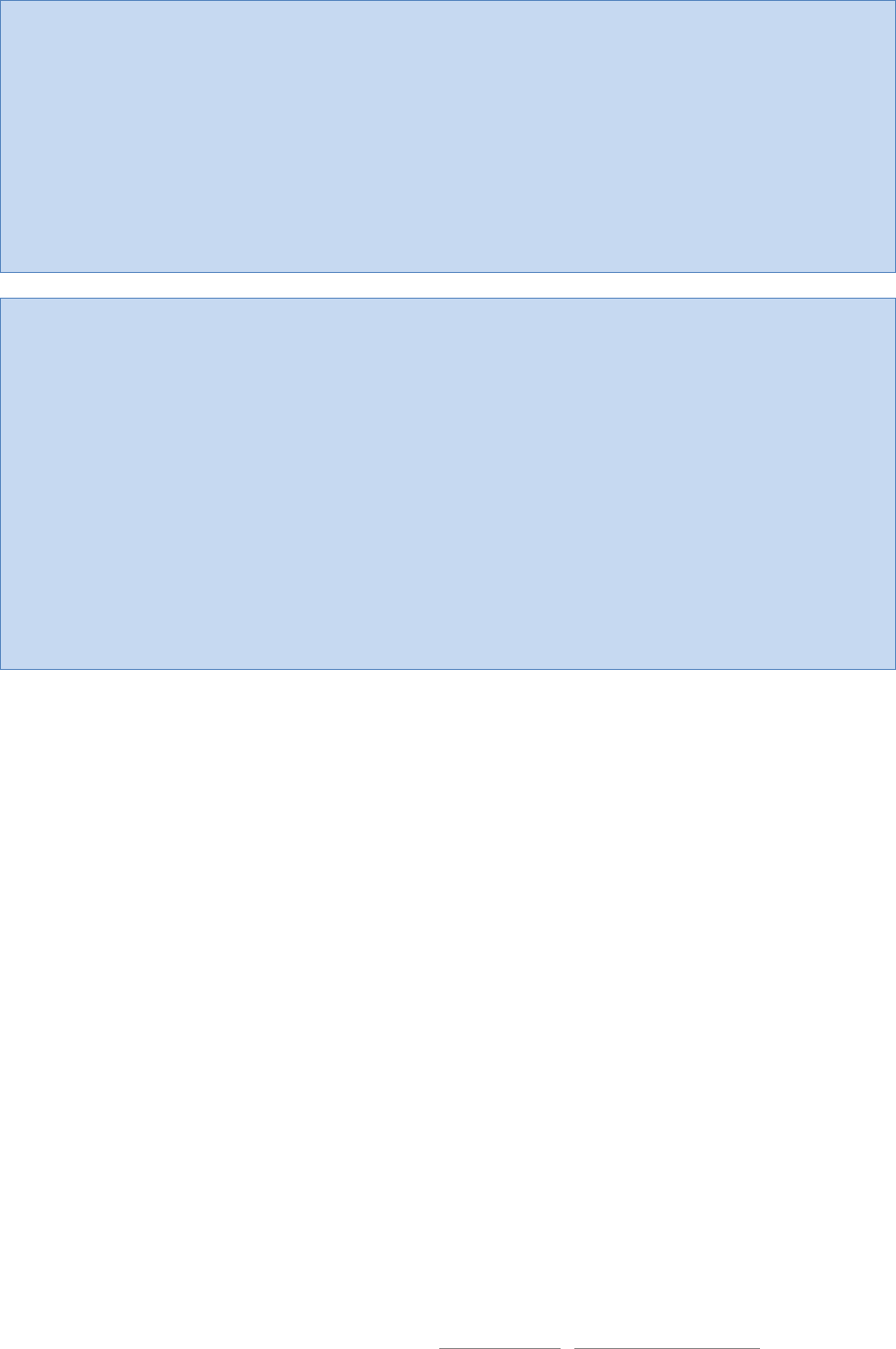
0
100
200
300
400
500
600
700
2016 compared to 2017
2016 2017
Issues in this bulletin
- Complaint statistics
- Ambulance bill complaints
- Lifetime Health Cover
- Top five complaint issues

© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
Ambulance cover complaints
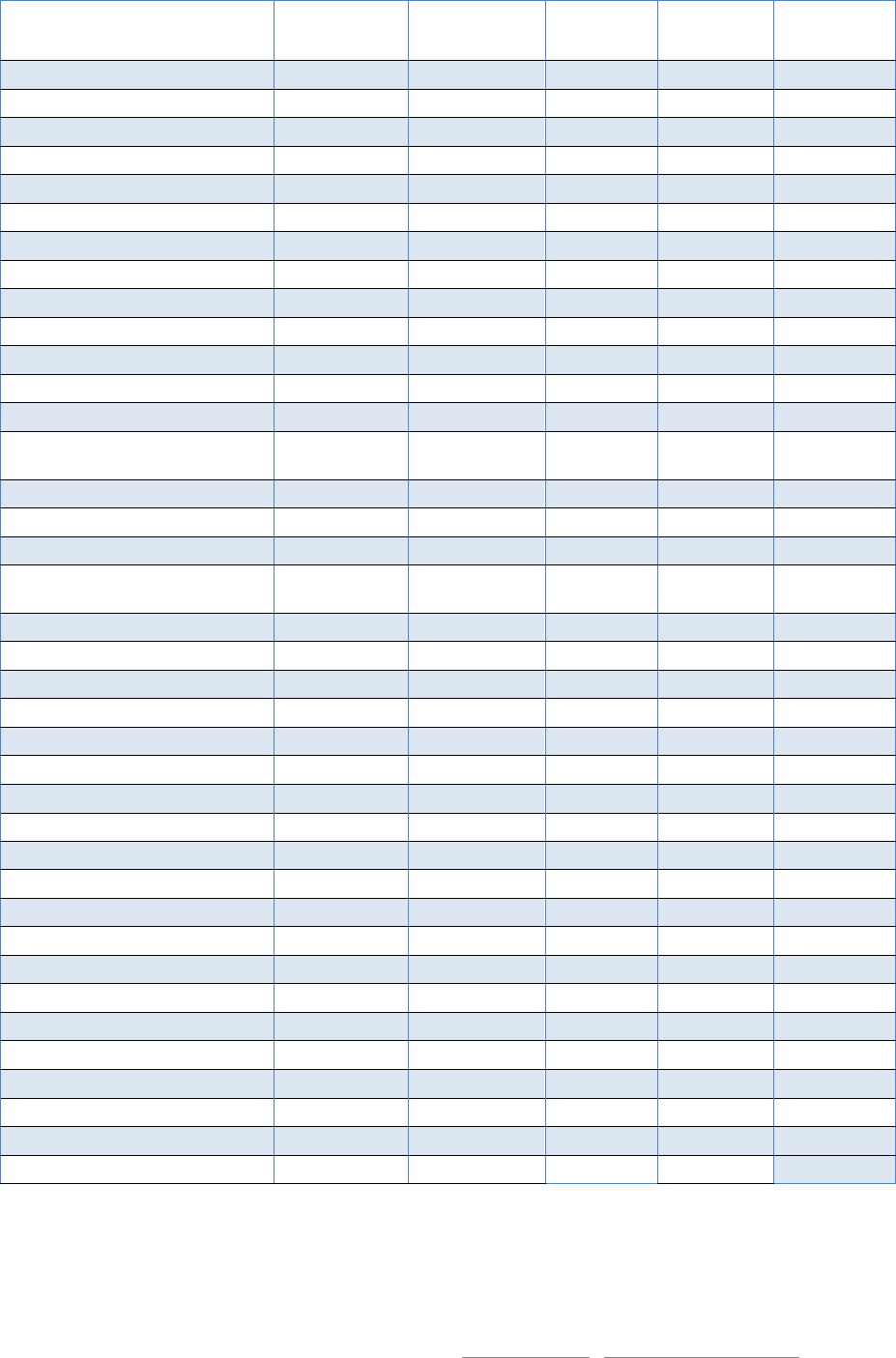
One area of complaints that has been increasing is ambulance cover complaints.
Ambulance costs in Australia are covered by a mix of government-regulated and private health insurance
arrangements. For a consumer seeking cover for ambulance costs, the Office recommends they carefully
consider the following questions, in addition to standard health insurance considerations:
Will the policy cover me when I'm travelling interstate?
Does the policy cover emergency situations only, or will it cover non-emergency as well? How
does the fund define an emergency?
What types of ambulance transport will this cover—for example, will it cover air ambulance? Will
it cover transport provided by state-approved private providers or other private providers?
Will the policy cover me for the ambulance 'call-out' fee if I need ambulance treatment but don't
require transportation?
Will I need to make any co-payments towards the ambulance fee?
It is perhaps not surprising that some health insurance consumers find it difficult to understand their health
insurance cover for ambulance given that the policy varies depending on where they are in Australia, what
‘code’ the ambulance service uses to categorise their service, who owns the ambulance and where they are
transported. It is understandable that some consumers feel that if they have a genuinely urgent need for
treatment and hold ambulance cover or a subscription they will be covered—unfortunately, there are some
instances where policy exclusions mean they are not covered.
Case study one
Willis, a resident of New South Wales, was on holiday in the Northern Territory visiting Alice Springs and
the surrounding area. On a very hot day, while near Alice Springs, he suffered dehydration and sunstroke.
Due to the limited medical facilities in Alice Springs and the vast distance to public hospitals, Willis was
transported by the Royal Flying Doctor Service’s air ambulance to a public hospital in South Australia.
His health insurer received his claim for the ambulance transport but refused to pay telling him that he
had used an ‘unrecognised provider’. Willis’ policy was one that covered recognised ambulance services,
including air ambulance services, throughout Australia. However it seemed that his insurer did not
recognise any air ambulance providers in the Northern Territory, and only recognised providers of road-
based ambulance transport in the vicinity of the two metropolitan cities.
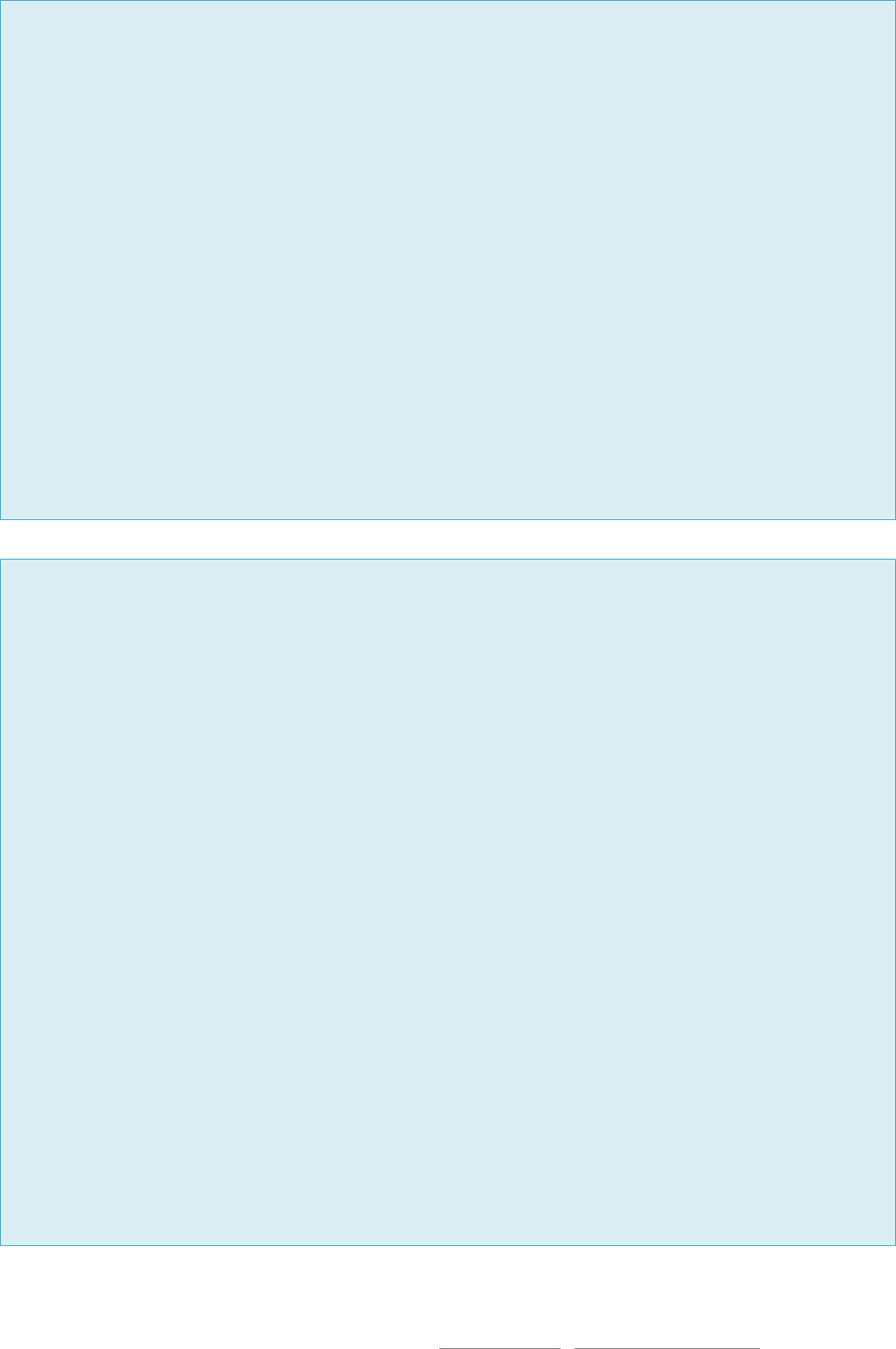
0
10
20
30
40
50
60
70
80
90
100
2007-08 2008-09 2009-10 2010-11 2011-12 2012-13 2013-14 2014-15 2015-16 2016-17
Ambulance cover complaints by year
© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
Willis contacted our Office to complain because he felt he had been given no choice of ambulance
provider at the time he sought medical help. He also felt that he had taken a policy that included
ambulance cover throughout Australia, but it didn’t cover most of the Northern Territory because the
insurer did not recognise the only air ambulance provider in that state.
Our investigation showed that Willis’ policy did indeed offer to cover him for ambulance throughout
Australia. It was therefore reasonable for a policyholder to expect that the insurer had ensured that it had
sufficient recognised ambulance providers throughout the country. Based on this view, the insurer
decided to pay Willis’s ambulance bill and to review its ambulance policy.
Case study two
Zelda broke her leg and ankle when she was out bushwalking in regional Victoria. On Monday, she was
taken to the nearest public hospital by ambulance. She was then transported to a private hospital and
received treatment within the hour. A week later, on Sunday, Zelda experienced post-operative
complications and called the ambulance to be transported to the nearest hospital.
Zelda’s policy was limited to two ambulance claims per year. Initially, the insurer refused to pay the most
recent service because they considered Zelda’s first service on Monday to be two claims—the trip to the
public hospital and then the transport to the private hospital.
In the Office’s view, this wasn’t reasonable as from Zelda’s perspective she had only been treated after
being transported to the second hospital and therefore this was one claim. After reviewing the case, the
health fund agreed to treat the first two transfers as one claim and also paid for the Sunday claim.
Hospital to hospital ambulance issues
Many of the ambulance bill complaints that our Office investigates seem to occur where there is some
ambiguity about who is responsible for paying an ambulance transport bill, or whether it should be issued in
the first place. For example, if a small regional hospital admits a patient who arrives by emergency
ambulance only to transfer them to a larger metropolitan hospital, then an ambulance account is usually
paid for by the ‘losing’ hospital that couldn’t treat the patient.
If, however, the losing hospital doesn’t formally admit the patient and instead treats them as an outpatient,
they can avoid paying the ambulance account because they no longer consider it a ‘hospital to hospital’
transfer. If a hospital chooses not to admit a patient and instead books a second ambulance to send them to
another hospital, the ambulance bill becomes the responsibility of the patient to pay.
The problem for health insurance consumers is that all ambulance policies exclude hospital to hospital
transfers and most won’t pay for non-emergency transport either. In some instances, consumers are
incurring costs of up to $5,000 when they are treated on an outpatient basis by a local hospital which then
transfers them to another hospital.
Issuing a patient with an ambulance bill is a concerning practice for a number of reasons:
Patients who make the effort to pay for health insurance ambulance cover consider it is unfair to be
charged due to gaps existing in the system. Although there are not many instances of this type of
failure in the system occurring, for the unlucky few, the out-of-pocket costs can be considerable.
© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
Treatment provided during the process of transporting a patient to one hospital and then forwarding
them to another hospital is likely to be seen as a ‘hospital to hospital’ admission by the patient
because they are physically present in the hospital. The distinction between outpatient and inpatient
treatment is, from their perspective, only an administrative detail.
It has long been the practice that hospitals that are unable to treat a patient that is brought to them
by ambulance look after the booking and costs of forwarding that patient to another hospital, so
these costs usually come as a surprise to patients.
Many of these complaints are resolved by pointing out that the system should not allow hospital bills to
become the complainant’s responsibility. Fully insured patients and anomalous accounts can be shared
between hospitals and health insurers on a case-by-case basis. Fortunately the number of patients being
billed for ambulance services in this manner is low.
The private health insurance system is not currently designed to pay for hospital to hospital transfers. Our
Office will continue monitoring these complaints and discuss our concerns with the public hospitals,
ambulance providers and health insurers involved.
Lifetime Health Cover
The Lifetime Health Cover (LHC) rules determine how much a person pays for Australian hospital insurance.
A person’s LHC ‘loading’ is the extra amount they pay on top of the base premium if they have missed their
window to purchase hospital insurance at the base rates. The current rules are contained in the Private
Health Insurance Act 2007 (Cth).
Due to the complexity of the rules, LHC is one of the most common topics that consumers raise when they
contact our Office. Health insurers also contact our Office from time to time to seek clarification.
Health insurer staff and health insurer websites should incorporate appropriate LHC questions into the join
or transfer process, so that a person’s LHC can be established as quickly and accurately as possible. Some
important questions to ask new members include:
Has the person held hospital insurance in Australia before and if so, when?
Are they a new migrant?
o If so, when did they enrol for their first interim or permanent Medicare card? (Note that a
person with reciprocal Medicare is not liable to pay LHC loading.)
Has the person been overseas for any extended periods and if so, when?
If necessary, ask the person to supply clearance certificates from their previous insurers and an
International Movement record from the Department of Home Affairs, to establish their loading.
Below we outline three LHC scenarios which are frequently raised by consumers and insurers contacting our
Office for assistance:
New migrant to Australia, overseas on their base day on or after 1 July 2010
Generally, a person must hold private hospital insurance by the later of the 1 July following their 31
st
birthday or 1 July 2000 to avoid incurring LHC loading. However, some exemptions do exist for certain
groups. New migrants who are aged over 31 have until the first anniversary of their first Medicare
enrolment to take up private hospital insurance without loading. Furthermore, if they enrolled in Medicare
from 1 July 2009 onwards, then they are eligible for a further extension if they are overseas on their
Medicare anniversary day.
© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
Yuna came to Australia on a working visa and later applied for permanent residency. On receiving her
bridging visa in 2015, she became eligible for Medicare and enrolled for an interim Medicare card in June
2015. She was then aged 35.
New migrants usually have 1 year from their first Medicare enrolment (at either an interim or permanent
level) to take up private hospital cover without incurring LHC loading. So this would place Yuna’s usual LHC
‘base day’ at June 2016. However, Yuna was actually living overseas for the period from April 2016
through to August 2017. She was therefore eligible for an extension as she was overseas on her base day.
The LHC rules state that if a new migrant is overseas on their base day, and their base day falls on or after
1 July 2010, then a further extension applies. They have one year from their first permanent return to
Australia to take up insurance without incurring a loading. Their ‘first permanent return’ is their first visit
back to Australia of 90 days or more.
Yuna returned in August 2017, so she has until August 2018 to take up insurance without loading. She will
need to supply her insurer with a Medicare letter confirming her enrolment date to establish her original
LHC base day and an International Movement record from the Department of Home Affairs, to establish
that she was overseas on the base day and first returned in August 2017.
If Yuna misses the August 2018 extension, even if she is overseas again at that date, no further
exemptions apply. A full loading based on her age at the time of joining will apply if she joins after August
2018.
The 10 year rule and ‘days of absence’
Under the LHC rules, a person’s loading is removed if they complete 10 years of hospital cover. They can
break up the 10 years using the ‘permitted periods without hospital cover’ as outlined in section 34–20 of
the Act. However, if the person subsequently drops their hospital insurance again and then picks it up at a
later time, having used up all their permitted periods, then they will incur their previous loading back again
as well as any further loading that has since accrued.
Ethan commenced hospital insurance at age 35 in 2002, incurring a 10 per cent loading. He completed 10
years of hospital cover in 2012, and his loading was subsequently reduced to zero. He continued his cover
for two more years. At age 47 in 2014, he cancelled his hospital insurance.
On cancelling his insurance, Ethan had access to the usual permitted periods without hospital cover which
are: suspension, going overseas for at least 12 months, and 1,094 ‘days of absence’ (three years less one
day). He did not suspend his insurance or go overseas for an extended period, so his time without
insurance was deducted from his 1,094 days of absence.
In 2017, he used up his full 1,094 days of absence.
In 2018, he re-joined private hospital insurance. He had used up his 1,094 days of absence, so two per
cent loading had accrued for the one further year he was without cover after the days of absence expired.
In addition to this, he re-gained his previous loading of 10 per cent.
Therefore his total loading on re-joining in 2018 was 12 per cent. Ethan needs to complete a further 10
years of continuous hospital insurance to reduce his loading to zero again.
It’s important to note that he has no further days of absence. If Ethan has even a small break of one day in
future (e.g. switching between insurers), this will potentially cause him to have to re-start his 10 years
again. The only time he can be without insurance and still have continuity of the 10 years will be if he
suspends his insurance or goes overseas for a period of at least 12 months.
© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
Australian, over 31, and overseas on 1 July 2000
There is one specific LHC exemption for Australians who were aged over 31 and were living overseas on
1 July 2000 which is different from almost all other exemptions. These individuals are able to return to
Australia and access the 1,094 days of absence, even though they have not previously held private hospital
cover.
Anaya departed Australia in 1998 to live overseas. She was aged 40 when she departed. Over the next
twelve years, she returned to Australia from time to time, mostly for short visits but including one long
visit of 12 months in 2007–08.
In 2010, she returned to Australia permanently, she was then aged 52. In 2017, at age 59, she purchased
private hospital cover.
Initially her insurer applied a LHC loading of 58 per cent, based on her age in 2017. However, there is a
specific LHC clause which provides a different outcome for people who were Australians or permanent
residents on 1 July 2000 who were also aged over 31 and overseas on that date. People who meet this
specific criteria are ‘taken to have had hospital cover’ on their LHC base day and therefore have access to
all the usual permitted periods without hospital cover.
This means they are considered to have zero loading at 1 July 2000. Any subsequent periods of time spent
overseas for 12 months or more do not count towards LHC loading, and any returns to Australia are
deducted from the 1,094 days of absence. Once the 1,094 days have been used up, the person
accumulates two per cent loading for each further year without hospital cover.
For Anaya, this means she had zero loading on her base day of 1 July 2000. It remained at zero for the
period from 1 July 2000 to her return in 2007 as she was overseas for a period of 12 months or more,
which is a permitted period without hospital cover.
In 2007 she returned for a period of 12 months. Her loading remained at zero, but this period is deducted
from her 1,094 days (three years less one day) of absence.
She went back overseas and her loading stayed at zero as the period was 12 months or more.
She returned in 2010. From 2010 onwards she began to use up the remaining two years of her 1,094 days
of absence, with the days of absence expiring in 2012. From 2012 onwards she began to accumulate two
per cent loading for each further year without hospital insurance.
By the time she joined in 2017, she had accumulated 12 per cent LHC loading.
Anaya then produced her International Movement record, showing her entries and exits from Australia,
and asked the insurer to review her LHC loading. Her insurer corrected the loading to 12 per cent and
refunded the excess she had paid in premiums. If Anaya completes 10 continuous years of private hospital
cover, her loading will be reduced to zero.
Further Resources:
The Office’s website privatehealth.gov.au includes the following resources:
LHC Calculators
Information on LHC
LHC brochure available in several community languages.
In the first instance, consumers should speak to their insurer for more advice. If they require further
assistance, they can contact our Office directly for more information on our enquiries line 1300 737 299 or at
© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
phio.info@ombudsman.gov.au. If a consumer wishes to lodge a complaint against their insurer, they can call
our complaints line 1300 362 072 or complete the online complaints form at ombudsman.gov.au.
Insurer staff seeking further advice should first contact the compliance or training staff in their organisation.
For complex queries, our Office can be contacted at phio.in[email protected]ov.au.
Top five consumer complaint issues this quarter
1. Hospital exclusions and restrictions: 105 complaints—usually caused when complainants find they
are not covered for a service or treatment that they had assumed was included in their cover.
2. General treatment (extras/ancillary): 77 complaints—these complaints usually concern disputes
over the amount payable under ‘extras’ policies, such as dental, optical, physiotherapy, and
pharmaceuticals, or the insurer’s rules for benefit payments (such as certain minimum claim
criteria).
3. Membership cancellation: 76 complaints—complaints caused by problems and delays associated
with processing requests to cancel memberships and handling payments or refunds. It’s important
to note that in most cases these membership cancellations are caused by consumers transferring
from one insurer to another and not the result of people leaving health insurance altogether.
4. Pre-existing conditions waiting period: 75 complaints—these complaints are usually caused by the
health insurer or the insurer’s medical practitioner failing to clearly state which signs and symptoms
were relied upon in assessing a claim and the complainant misunderstanding how a pre-existing
condition is defined.
5. Verbal advice: 64 complaints—most verbal advice complaints concern consumers misunderstanding
their benefits during telephone calls and retail branch visits with their insurer, particularly where
records are not adequately maintained. In many cases our case officers will access the recording of
advice provided to a consumer and provide an independent assessment of the quality of the
information provided.
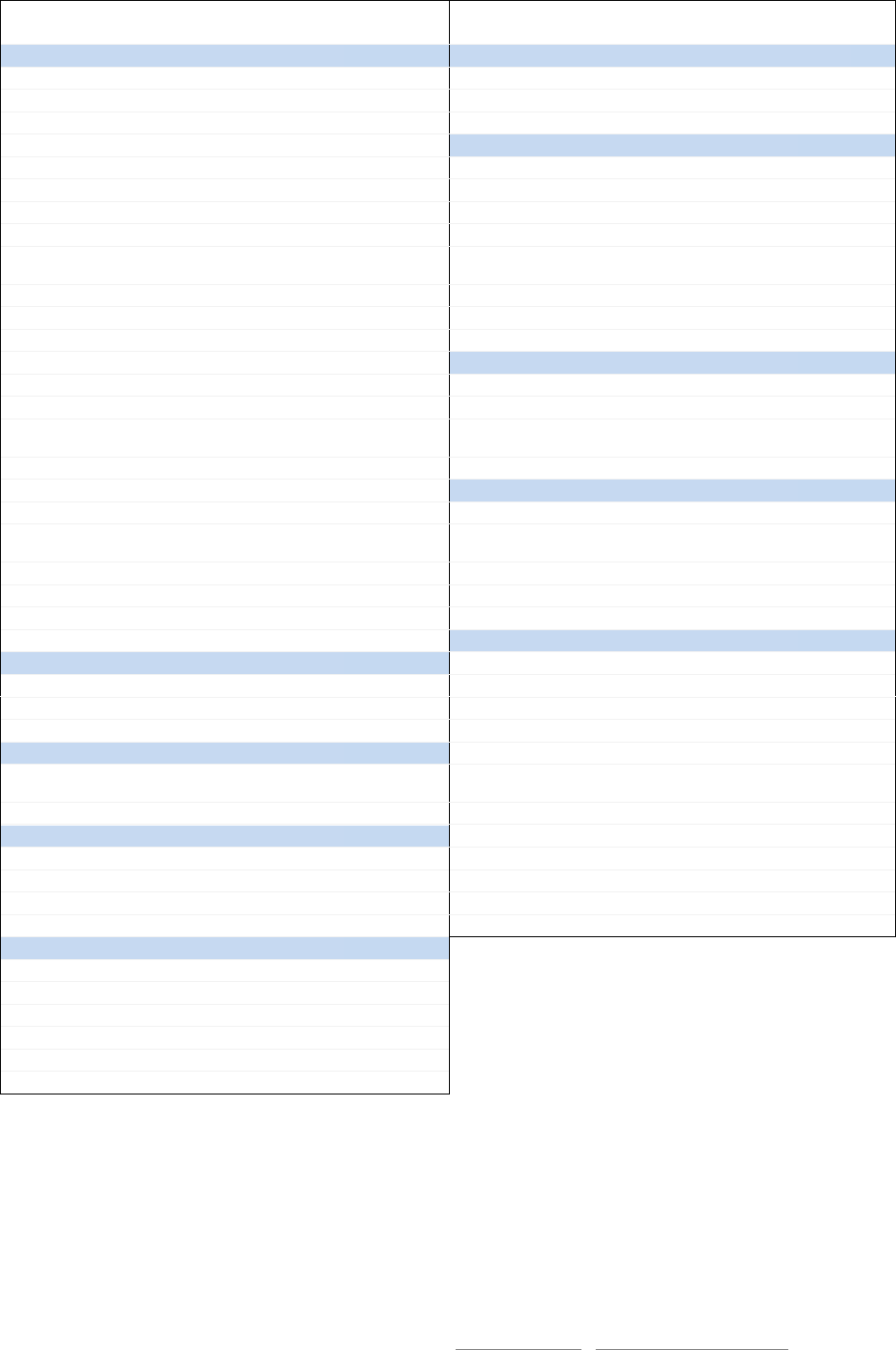
Complaints by provider or organisation type
Provider or organisation type
Mar 2017
QTR
Jun 2017 QTR
Sep 2017 QTR
Dec 2017 QTR
Health insurers
1,245
1,237
1,020
780
Overseas visitor & overseas student
health Insurers
108
114
141
114
Brokers and comparison services
19
25
26
17
Doctors, dentists, other medical
providers
6
13
4
3
Hospitals and area health services
15
17
13
15
Other (e.g. legislation, ambulance
services, industry peak bodies, etc.)
19
25
18
11

© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
Subscribe for updates
To be added to our distribution list for private health insurance news and publications, sign up using our
online form or email phio.info@ombudsman.gov.au.
You can also follow us on Facebook for updates: facebook.com/commonwealthombudsman/
For general private health insurance information and to compare health insurance policies, visit
privatehealth.gov.au
© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
Complaints by health insurer market share
1 October to 31 December 2017
Name of Insurer
Complaints(1)
Percentage of
complaints
Disputes(2)
Percentage
of disputes
Market
share(3)
ACA Health Benefits
0
0.0%
0
0.0%
0.1%
Australian Unity
49
6.3%
8
6.8%
3.0%
BUPA
222
28.5%
48
41.0%
27.0%
CBHS Corporate Health
0
0.0%
0
0.0%
<0.1%
CBHS
12
1.5%
1
0.9%
1.5%
CDH (Cessnock District Health)
0
0.0%
0
0.0%
<0.1%
CUA Health
7
0.9%
1
0.9%
0.6%
Defence Health
4
0.5%
0
0.0%
2.0%
Doctors' Health Fund
2
0.3%
0
0.0%
0.3%
Emergency Services Health
0
0.0%
0
0.0%
<0.1%
GMHBA
23
2.9%
2
1.7%
2.3%
Grand United Corporate Health
5
0.6%
0
0.0%
0.4%
HBF Health & GMF/Healthguard
38
4.9%
5
4.3%
8.0%
HCF (Hospitals Contribution
Fund)
111
14.2%
20
17.1%
10.4%
Health.com.au
11
1.4%
5
4.3%
0.6%
Health Care Insurance
1
0.1%
0
0.0%
0.1%
Health-Partners
2
0.3%
0
0.0%
0.6%
HIF (Health Insurance Fund of
Aus.)
7
0.9%
1
0.9%
0.9%
Latrobe Health
3
0.4%
0
0.0%
0.7%
Medibank Private & AHM
183
23.5%
12
10.3%
26.9%
Mildura District Hospital Fund
0
0.0%
0
0.0%
0.2%
MO Health Pty Ltd
0
0.0%
0
0.0%
<0.1%
National Health Benefits Aust.
0
0.0%
0
0.0%
0.1%
Navy Health
1
0.1%
0
0.0%
0.3%
NIB Health
62
7.9%
7
6.0%
8.3%
Nurses and Midwives Pty Ltd
1
0.1%
0
0.0%
<0.1%
Peoplecare
7
0.9%
1
0.9%
0.5%
Phoenix Health Fund
1
0.1%
1
0.9%
0.1%
Police Health
0
0.0%
0
0.0%
0.3%
QLD Country Health Fund
1
0.1%
0
0.0%
0.4%
Railway & Transport Health
7
0.9%
2
1.7%
0.4%
Reserve Bank Health
0
0.0%
0
0.0%
<0.1%
St Lukes Health
0
0.0%
0
0.0%
0.5%
Teachers Federation Health
16
2.1%
2
1.7%
2.3%
Teachers Union Health
2
0.3%
0
0.0%
0.6%
Transport Health
1
0.1%
0
0.0%
0.1%
Westfund
1
0.1%
1
0.9%
0.7%
Total for Health Insurers
780
100%
117
100%
100%
1) Total number of Complaints (Problems, Grievances & Disputes) regarding Australian registered health insurers. This table excludes
complaints regarding OVHC and OSHC insurers, and other bodies.
2) Disputes required the intervention of the Ombudsman and the health insurer.
3) Source: Australian Prudential Regulation Authority, Market Share, All Policies, 30 June 2017.
© Commonwealth Ombudsman | 1300 362 072 | ombudsman.gov.au | phio.info@ombudsman.gov.au
Issues and sub-issues: complaints received in previous four quarters
ISSUE
Mar
17
Jun
17
Sep
17
Dec
17
ISSUE
Mar
17
Jun
17
Sep
17
Dec
17
Sub-issue
Sub-issue
BENEFIT
INFORMED FINANCIAL CONSENT
Accident and emergency
10
10
20
16
Doctors
7
7
1
0
Accrued benefits
2
3
1
2
Hospitals
10
17
9
12
Ambulance
17
21
16
21
Other
0
3
2
1
Amount
51
54
32
17
MEMBERSHIP
Delay in payment
54
70
43
28
Adult dependents
5
9
7
1
Excess
22
16
17
21
Arrears
31
14
23
14
Gap - Hospital
22
23
13
25
Authority over membership
3
3
3
8
Gap - Medical
33
29
25
33
Cancellation
97
111
97
76
General treatment
(extras/ancillary)
52
36
59
77
Clearance certificates
41
57
50
18
High cost drugs
4
2
1
3
Continuity
47
44
31
18
Hospital exclusion/restriction
73
90
120
105
Rate and benefit protection
4
9
1
0
Insurer rule
38
30
27
24
Suspension
23
22
26
15
Limit reached
6
4
14
3
SERVICE
New baby
6
6
8
3
Customer service advice
32
53
41
19
Non-health insurance
5
1
0
2
General service issues
81
65
55
42
Non-health insurance - overseas
benefits
0
0
0
0
Premium payment problems
127
163
57
36
Non-recognised other practitioner
6
9
4
2
Service delays
60
45
21
18
Non-recognised podiatry
4
5
1
1
WAITING PERIOD
Other compensation
3
6
7
3
Benefit limitation period
0
0
1
0
Out of pocket not elsewhere
covered
9
5
5
6
General
6
6
10
9
Out of time
5
3
4
10
Obstetric
7
11
9
9
Preferred provider schemes
19
15
11
9
Other
4
6
6
3
Prostheses
1
5
0
2
Pre-existing conditions
59
88
93
75
Workers compensation
1
2
1
0
OTHER
CONTRACT
Access
1
0
0
0
Hospitals
10
4
8
2
Acute care certificates
1
3
1
2
Preferred provider schemes
2
8
6
5
Community rating
0
0
1
0
Second tier default benefit
1
1
0
0
Complaint not elsewhere covered
24
24
14
10
COST
Confidentiality and privacy
4
2
4
2
Dual charging
4
0
0
0
Demutualisation/sale of health
insurers
1
0
0
1
Rate increase
95
32
8
4
Discrimination
0
0
0
0
INCENTIVES
Medibank sale
1
0
1
0
Lifetime Health Cover
46
63
55
27
Non-English speaking background
0
0
0
0
Medicare Levy Surcharge
1
2
4
2
Non-Medicare patient
2
3
3
0
Rebate
9
11
4
3
Private patient election
3
2
1
0
Rebate tiers and surcharge changes
2
0
0
1
Rule change
33
14
6
0
INFORMATION
Brochures and websites
16
15
12
6
Lack of notification
11
15
15
19
Oral advice
80
87
91
64
Radio and television
1
0
0
0
Standard Information Statement
1
1
3
0
Written advice
21
8
9
6
