
Substance Abuse and Mental Health
Services Administration
Harm Reduction
Framework

Public Domain Notice
All material appearing in this publication is in the public domain and may be reproduced or
copied without permission from SAMHSA. Citation of the source is appreciated. However,
this publication may not be reproduced or distributed for a fee without the specific, written
authorization of the Office of Communications, SAMHSA, HHS.
Electronic Access and Copies
Products may be downloaded at https://www.samhsa.gov/find-help/harm-reduction/
framework
Recommended Citation
Substance Abuse and Mental Health Services Administration: Harm Reduction Framework.
Center for Substance Abuse Prevention, Substance Abuse and Mental Health Services
Administration, 2023.
Originating Office
Center for Substance Abuse Prevention, Substance Abuse and Mental Health Services
Administration, 5600 Fishers Lane, Rockville, MD 20857.
Nondiscrimination Notice
The Substance Abuse and Mental Health Services Administration (SAMHSA) complies with
applicable Federal civil rights laws and does not discriminate on the basis of race, color,
national origin, age, disability, religion, or sex (including pregnancy, sexual orientation,
and gender identity). SAMHSA does not exclude people or treat them differently because
of race, color, national origin, age, disability, religion, or sex (including pregnancy, sexual
orientation, and gender identity).

Harm Reducon Framework
3
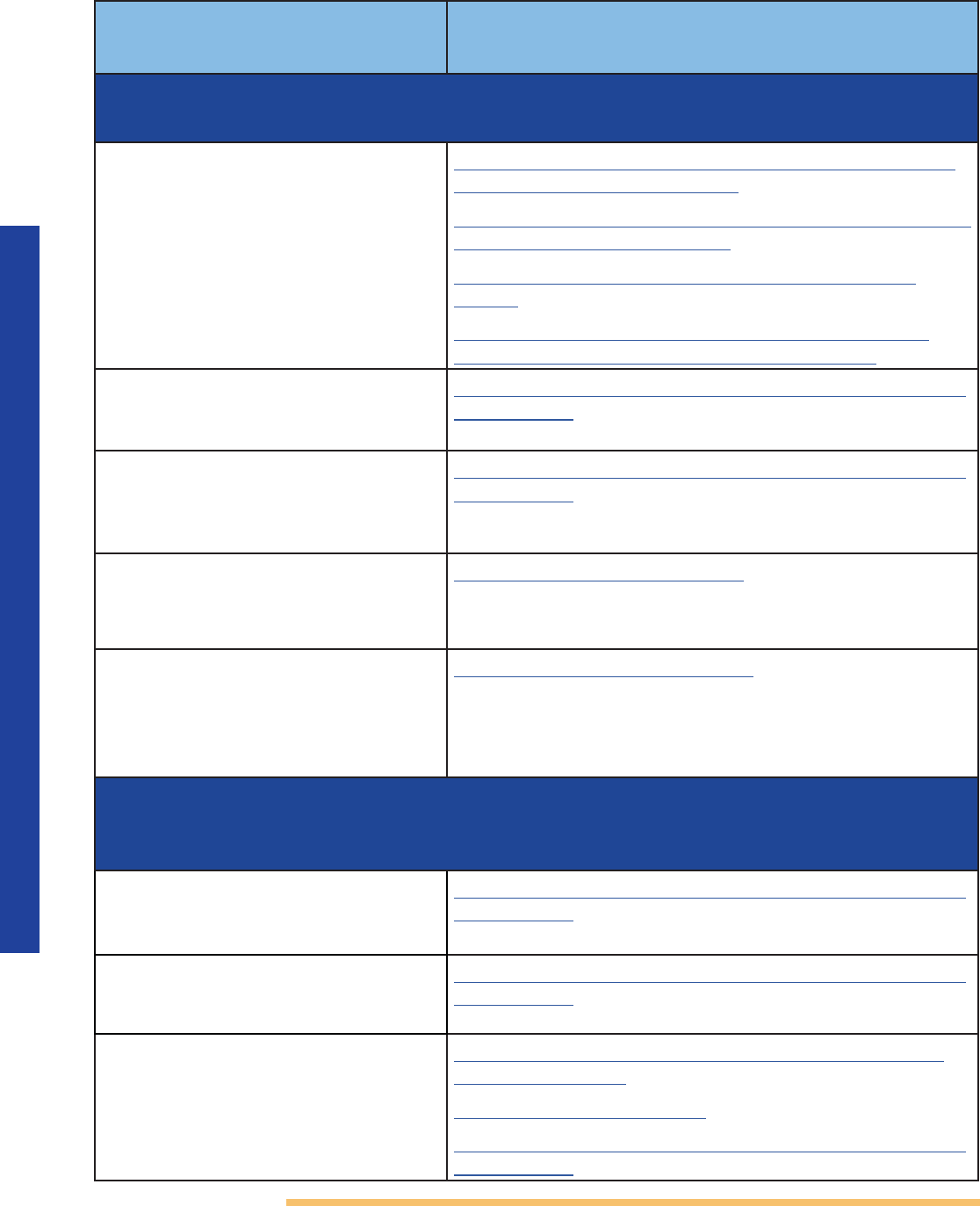
Contents
Harm Reduction Framework for People Who Use Drugs (PWUD) ...................................................... 4
Brief History and Background of Harm Reduction
........................................................................................5
Addressing Health Inequities
......................................................................................................................................... 6
Framework Overview
.......................................................................................................................................................... 6
• Framing Harm Reduction.................................................................................................................................7
• Pillars of Harm Reduction .................................................................................................................................8
• Table 1. Six Pillars of Harm Reduction .......................................................................................................8
• Supporting Principles ........................................................................................................................................10
• Table 2. Principles of Harm Reduction ................................................................................................... 10
• Core Practice Areas.................................................................................................................................................. 12
• Table 3. Core Practice Areas ........................................................................................................................... 12
• Community-Based Harm Reduction Programs (CHRPs) ......................................................... 17
Conclusion
............................................................................................................................................................................ 17
References
............................................................................................................................................................................18
Harm Reduction Steering Committee Members
......................................................................................... 25

Harm Reducon Framework
4
Harm Reduction Framework for People Who
Use Drugs (PWUD)
The Biden-Harris Administration has identified harm reduction as a federal drug policy
priority. The White House Office of National Drug Control Policy (ONDCP), in the 2022
National Drug Control Strategy, notes that harm reduction is a public health approach
designed to advance policies and programs in collaboration with people who use drugs
(PWUD) and is supported by decades of evidence. Harm reduction strategies are shown to
substantially reduce HIV and hepatitis C infection among people who inject drugs, reduce
overdose risk, enhance health and safety, and increase by five-fold the likelihood of a person
who injects drugs to initiate substance use disorder treatment.
1, 2, 3
In line with this, harm
reduction is one of the four strategic priorities of the U.S. Department of Health and Human
Services (HHS) Overdose Prevention Strategy developed to address the overdose public
health emergency.
4
In December 2021, the Substance Abuse and Mental Health Services Administration
(SAMHSA) convened the first-ever federal Harm Reduction Summit, in partnership with
the Centers for Disease Control and Prevention (CDC) and ONDCP. The Summit brought
together more than 100 experts representing prevention, treatment, recovery, and harm
reduction perspectives. Most importantly, Summit attendees included people with lived
experience with substance use to help inform SAMHSA’s policies, programs, and practices
as they relate to harm reduction. Additional partners included community members,
advocates, harm reductionists, providers, funders, and others who are affected by these
issues.
SAMHSA’s Harm Reduction Framework is one outcome of the Summit. This Framework is
historic, as the first document to comprehensively outline harm reduction and discuss its
role throughout HHS.
The Framework was developed and written in partnership with the Harm Reduction
Steering Committee, composed of harm reduction leaders in the field from across the
country. This group represents a broad array of backgrounds and experience, with most
having lived experience of drug use. The Steering Committee synthesized findings from the
Summit ― including a definition of harm reduction, pillars and principles supporting that
definition, and core practices that SAMHSA can support. The Framework is adapted from
the Committee’s final report.
This Framework will inform SAMHSA’s harm reduction activities moving forward, as well
as related policies, programs, and practices. SAMHSA’s aim is to integrate harm reduction
activities and approaches across its organizational Centers and initiatives, and to do so in
a manner that draws on evidence-based practice and principles ― while also maintaining
sustained dialogue with harm reductionists and people who use drugs (PWUD). The
Framework will also inform SAMHSA’s thinking about opportunities to work with other
federal, state, tribal, and local partners toward advancing harm reduction approaches,
services, and programs.
SAMHSA defines harm reduction as a practical and transformative approach that
incorporates community-driven public health strategies — including prevention,
risk reduction, and health promotion — to empower PWUD and their families
with the choice to live healthier, self-directed, and purpose-filled lives. Harm
reduction centers the lived and living experience of PWUD, especially those in
underserved communities, in these strategies and the practices that flow from them.

Harm Reducon Framework
5
Brief History and Background of Harm
Reduction
Harm reduction has a long history in the United States. The field itself and harm reduction
practice emerged decades ago, as direct community action and mutual aid in response
to effects of the “War on Drugs,” an early and incomplete scientific understanding of
substance use and substance use disorders, and government inaction to swiftly respond to
the growing HIV/AIDS epidemic.
5
In 1982, CDC published findings that the human immunodeficiency virus (HIV) is
transmissible through the intravenous use of drugs.
6
By 1983, PWUD began the
distribution of sterile syringes to limit the transmission of HIV/AIDS.
7
After the 1988
restriction on federal funding for the purchase of syringes for needle and syringe
exchange programs, PWUD and allies who operated syringe services programs
(SSPs) across the country began to organize their work.
8
In 1992, the first Harm
Reduction Working Group meeting in the United States was held in San Francisco to
create a unified definition of harm reduction. A major outcome of the group was the
establishment of the National Harm Reduction Coalition.
9
Since the first Harm Reduction Working Group meeting in 1992, harm reduction has
grown in scope and in practice. PWUD have innovated and sustained the movement
despite criminalization of many harm reduction interventions and lack of financial and
social support.
An important example is the advent of community naloxone distribution, which began
in 1996.
10
From 1996 through June 2014, 136 organizations reported distributing naloxone
to 152,283 laypersons. Of the 109 organizations who collect reversal data, 26,463 overdose
reversals were reported.
11
Although the number of organizations distributing naloxone
has doubled and since 2013 has included organizations other than SSPs, in 2014, SSPs
still accounted for 80 percent of the distribution effort to PWUD, as well as 80 percent of
overdose reversals.
12
In 2019, SSPs distributed 702,232 doses of naloxone to 230,506 people in communities
across the country.
13
Studies have shown that communities may experience up to a 46
percent reduction in opioid overdose mortality when more than 100 people who are likely
to observe or experience an overdose per 100,000 population are enrolled into an Overdose
Education and Naloxone Distribution (OEND) program.
14
In addition, SSPs are associated
with an estimated 50 percent reduction in HIV and hepatitis C incidence.
15,16
When
combined with medications that treat opioid use disorder (also known as medications for
opioid use disorder or MOUD), hepatitis C virus and HIV transmission is reduced by more
than two-thirds.
17
The last few decades have solidified the evidence-based practices and
individuals have become specialized subject matter experts in the field of harm reduction.

Harm Reducon Framework
6
Addressing Health Inequities
In the spirit of Executive Order 13985,
18
SAMHSA is in the process of reviewing its policies to
examine the intended and unintended impacts of its programs, policies, and procedures;
incorporating racial justice and health equity into its policy goals; and advancing equitable
support for Black, Latino, American Indian and Alaskan Native persons, Asian Americans,
Native Hawaiians, and Pacific Islanders, and other persons of color; members of religious
minorities; lesbian, gay, bisexual, transgender, queer, intersex (LGBTQI+) persons; persons
with disabilities; persons who live in rural areas; and persons otherwise adversely impacted
by persistent poverty or inequality. This is proactively undertaken to address past and
present inequities.
18
Integrating harm reduction principles and approaches throughout the
agency is one strategy for advancing that commitment.
Deficient social determinants of health and structural inequalities contribute to and
exacerbate substance use, substance use disorder, and mental illness, and can and do
have a profound impact on some populations. Most notably, persons who have a history of
familial, community or racial trauma may be particularly in need of compassionate services
to support their pathways to improved health outcomes. Community practitioners and
behavioral health providers must be culturally responsive and attentive to health equity
to effectively improve individual and population level health. For this to be accomplished,
community trust and buy-in must be earned, and that begins with truth and reconciliation
of a community’s shared traumatic history and the structural racism that perpetuates
inequities. On this foundation, trust and meaningful relationships can develop.
19
“Formally acknowledging a community’s shared
traumatic history is a fundamental step in preparing for
and planning community engagement (CE) efforts that
address health inequities.”
19
This work is undertaken in partnership with SAMHSA’s Office of Behavioral Health Equity,
which describes the work as: “Advancing health equity involves ensuring that everyone
has a fair and just opportunity to be as healthy as possible. This also applies not only to
behavioral health, but in conjunction with quality services, this involves addressing social
determinants, such as employment and housing stability, insurance status, proximity to
services, culturally responsive care — all of which have an impact on behavioral health
outcomes.”
20
Framework Overview
Harm reduction is practical in its understanding and acceptance that drug use and other
behaviors that carry risk exist ― and responds in a compassionate and life-preserving
manner. Harm reduction seeks to reduce the harmful impacts of stigma, mistreatment,
discrimination, and harsh punishment of PWUD, especially those who are Black,
Indigenous, and other People of Color.
21
Building community partnerships with harm
reduction organizations can positively shape beliefs and attitudes, reduce stigma, and
ensure the well-being of the community at large.
22

Harm Reducon Framework
7
Harm reduction also accounts for the intersection of drug use, other stigmatized behaviors,
and people’s health. Fundamentally, a harm reduction approach meets people where they
are, engaging with them and providing support.
23
Harm reduction opens the door to more options for PWUD, for whom traditional treatment
approaches are inaccessible, ineffective, or inappropriate — and who want to make safer,
healthier choices with their life and health. Access to harm reduction services is consistently
shown to improve individual and community outcomes. By viewing substance use on a
continuum, incremental change can be made, allowing for risk reduction to better suit a
person’s own individual goals and motivations.
Most importantly, harm reduction approaches save lives.
The SAMHSA definition of harm reduction contains six pillars, 12 principles, and six core
practice areas that give life to harm reduction approaches, initiatives, programs, and
services. The pillars are essential building blocks that are the foundation of what makes
harm reduction effective. The pillars are further divided into supporting principles that are the
specific concepts and ideals supporting each pillar. The SAMHSA Framework also describes
the core components of community-based harm reduction programs.
Framing Harm Reduction
SAMHSA conceptualizes harm reduction as being a set of services, an approach, and a
type of organization. Harm reduction has, at times, been reduced to a singular service or
group of services, when in fact, its application goes well beyond this. Harm reduction as
an approach — with supporting principles and pillars that can be applied to a variety of
contexts — includes the provision of evidence-based treatment. An organization or an
individual healthcare practitioner may not consider themselves as primarily providing
harm reduction services but may adopt and apply practices and principles outlined in this
Framework ― to enhance the services they offer and engage with PWUD in a manner
informed by these principles. Any organization who works with PWUD can benefit from the
integration of harm reduction as an approach.
Harm reduction is also part of the continuum of care and a comprehensive strategy that
includes prevention, treatment, recovery, and health promotion. All of these elements are
necessary — and people weigh them differently in different situations, at different points in
their lives, and relative to a wide range of substances and behaviors.
Prevention, in particular primary prevention, seeks to prevent problems before they start.
That means preventing exposure to substances (or screening and intervening with early
misuse), reducing risk factors, and strengthening protective factors at the individual,
relationship, community, and society levels. Prevention also seeks to stop or delay the
progression of substance use to a substance use disorder, as well as prevent other harms
associated with substance use.
Harm reduction recognizes the complex relationship people may have with substances,
starting from first use, through the many possible intervention points from there.
Harm reduction does not minimize the inherent harms associated with drug use and
acknowledges that reducing harm can take different forms for different people at different
points, including with the use of medications to treat substance use disorders. Harm
reduction is also inclusive of abstinence as a chosen pathway but not inclusive of abstinence
as a coerced pathway.
Harm Reducon Framework
8
Harm reduction services must adhere to the harm reduction approach to maintain fidelity
to the evidence base and lead to better outcomes. This is exemplified by the concept of
Community-Based Harm Reduction Programs (CHRPs) described in this Framework.
Pillars of Harm Reduction
Table 1 summarizes the six pillars of harm reduction. Harm reduction initiatives, programs,
or services should include these elements.
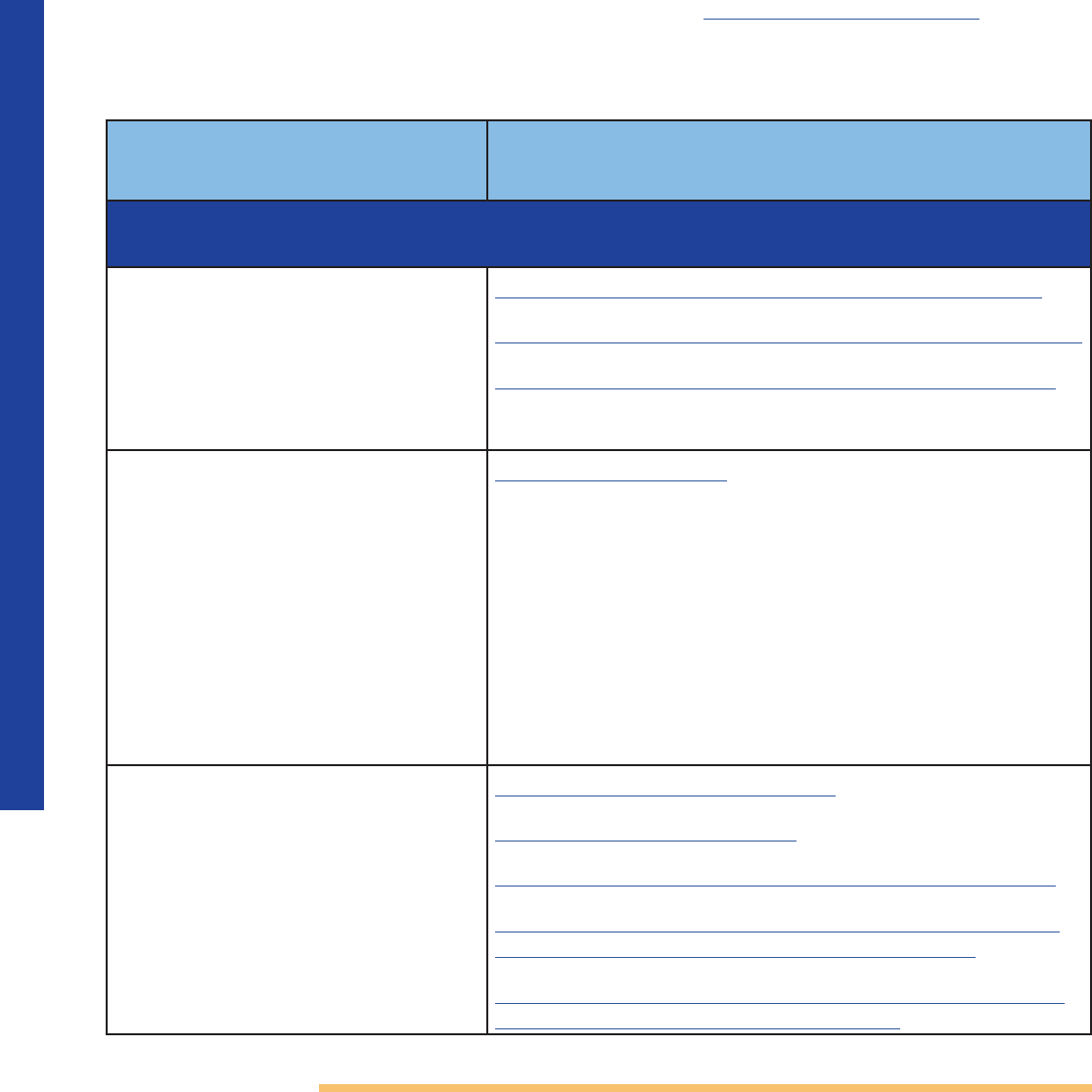
Table 1. Six Pillars of Harm Reduction
Harm Reduction...
1. Is led by people
who use drugs
(PWUD) and
with lived
experience of
drug use
Work is led by PWUD and those with lived and living experience
of drug use. Harm reduction interventions that are evidence
based have been innovated and largely implemented by PWUD.
Through shared decision-making, people with lived experience
are empowered to take an active role in the engagement process
and have better outcomes.
24
Put simply, the effectiveness of harm
reduction programs is based on the buy-in and leadership of the
people they seek to serve.
Organizations providing harm reduction services should have a
formal mechanism to meaningfully include the voices of people
with lived experience in the design, implementation, and evaluation
of those services.
25
Adopting at least two of the following specific
mechanisms of inclusion is mission critical: employment of people
with lived experience in both intervention and administrative roles,
advisory boards of PWUD, and the consultation of CHRPs or any
other peer-led organizations.
It is important to note that while people in recovery and people
who formerly used drugs have valuable experience, centering
the perspectives of people who currently use drugs (and the
intersectionality with other historically marginalized individuals) and
have a working understanding of the current, dynamic, and rapidly
changing landscape of drug use in a particular community in which
an organization is working, is essential to successful engagement
and outcomes. This is exemplified in the provision of OEND
Programs.
26
2. Embraces the
inherent value
of people
All individuals have inherent value and are treated with dignity,
respect, and positive regard.
Harm reduction initiatives, programs, and services are trauma
informed, and never patronize nor pathologize PWUD, nor their
communities. They acknowledge that substance use happens, and
the reasons a person uses drugs are nuanced and complex. This
includes people who use drugs to alleviate symptoms of an existing
medical condition.
Harm Reducon Framework
9
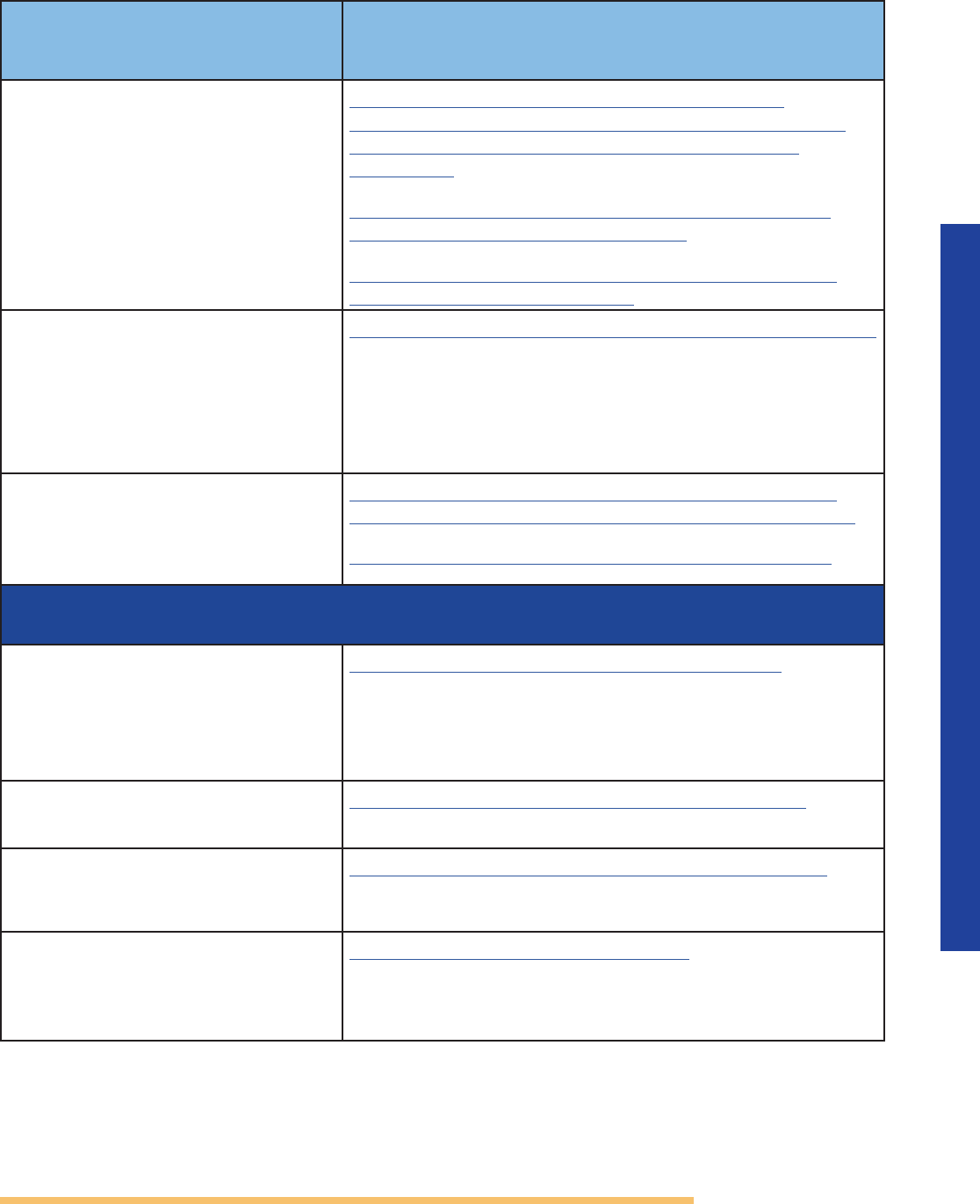
Harm Reduction...(Cont.)
3. Commits
to deep
community
engagement
and community
building
All communities that are impacted by systemic harms are leading
and directing program planning, implementation, and evaluation.
Funding agencies and funded programs support and sustain
community cultural practices, and value community wisdom and
expertise. Agencies and programs develop through community-
led initiatives focused on geographically specific, culturally
based models that integrate language revitalization, cultural
programming, and Indigenous care with dominant-society
healthcare approaches.
4. Promotes
equity, rights,
and reparative
social justice
All aspects of the work incorporate an awareness of (and actively
work to eliminate) inequity related to race, class, language, sexual
orientation, and gender-based power differentials.
Pro-health and pro-social practices that have worked well for specific
cultural and/or geographic communities are aligned with organizing
and mobilizing, providing direct services, and supporting mutual aid
among PWUD.
CHRPs are often the best-placed organizations to respond to
communities or individuals on racial justice and health equity
issues, and provide services for Black, Latino, American Indian and
Alaska Native persons, Asian Americans, Native Hawaiians, and
Pacific Islanders, and other persons of color; members of religious
minorities; LGBTQI+ persons; persons with disabilities; persons who
live in rural areas; and persons otherwise adversely impacted by
persistent poverty or inequality.
5. Offers most
accessible and
noncoercive
support
All harm reduction services have the lowest requirements for access.
Participation in services is always voluntary, confidential (or
anonymous), self-directed, and free from threats, force, and the
concept of compliance. Any data collection requires informed
consent and participants should not be denied services for not
providing information. This means using low-threshold evaluation
and data collection systems to measure the effectiveness of harm
reduction programs.
6. Focuses on any
positive change,
as defined by
the person
All harm reduction services are driven by person-centered positive
change in the individual’s quality of life.
Harm reduction initiatives, programs, and services recognize that
positive change means moving towards more connectedness to
the community, family, and a more healthful state, as the individual
defines it. There are many pathways to wellness; substance use
recovery is only one of them. Abstinence is neither required nor
discouraged.
Harm Reducon Framework
10
Table 2. Principles of Harm Reduction
Supporting
Principles
Principle Description
Respect
autonomy
Each individual is different. It is important to meet people where
they are, and for people to lead their own individual journey. Harm
reduction approaches, initiatives, programs, and services value and
support the dignity, personal freedom, autonomy, self-determination,
voice, and decision making of PWUD.
Practice
acceptance and
hospitality
Love, trust, and connection are important in harm reduction work.
Harm reduction approaches, initiatives, programs, and services hold
space for people who are at greatest risk for marginalization and
discrimination. These elements emphasize trusting relationships and
meaningful connections and understand that this is an important way
to motivate people to find personal success and to feel less isolated.
Provide support Harm reduction approaches, initiatives, programs, and services provide
information and support without judgment, in a manner that is
non-punitive, compassionate, humanistic, and empathetic. Peer-led
services enhance and support individual positive change and recovery;
and peer-led leadership leads to better outcomes.
Connect with
community
Positive connections with community, including family members
(biological or chosen) are an important part of well-being. Community
members often assist loved ones with safety, risk reduction, or
overdose response. When possible, harm reduction initiatives,
programs, and services support families in expanding and deepening
their strategies for love and support; and include families in services,
with the explicit permission of the individual.
Provide many
pathways to
well-being across
the continuum of
health and social
care
Harm reduction can and should happen across the full continuum
of health and social care, meeting whole-person health and social
needs. In networking with other providers, harm reduction initiatives,
programs, and services work to build relationships and trust with
health and social care partners that embrace supporting principles.
To help achieve this, organizations practicing harm reduction utilize
education and encourage policies that facilitate interconnectedness
between all parties.
Supporting Principles
The pillars are supported and reinforced by 12 core principles that guide the work. As with
the pillars, the principles are vital. Programs that do not incorporate all 12 principles risk
violating the spirit of harm reduction.
Harm Reducon Framework
11
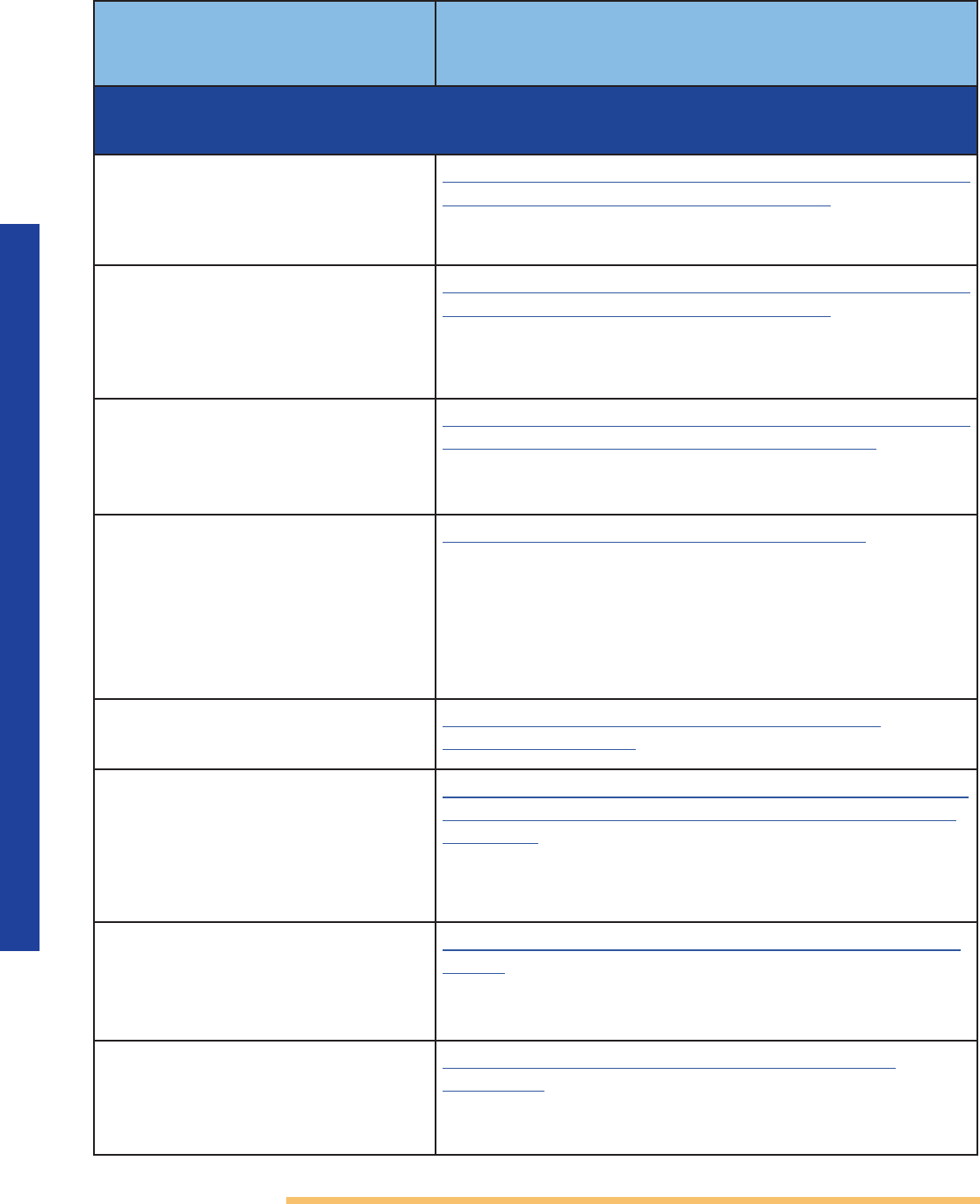
Supporting
Principles
Principle Description...(Cont.)
Value practice-
based evidence
and on-
the-ground
experience
Structural racism and other forms of discrimination have limited the
development and inclusion of research on what works in underserved
communities. Harm reduction initiatives, programs, and services
understand these limitations and use community wisdom and
practice-based evidence as additional sources of knowledge.
Cultivate
relationships
Relationships are of central importance to harm reduction. Harm
reduction approaches, initiatives, programs, and services are relational,
not transactional, and work to establish and support quality
relationships between individuals, families, and communities.
Assist, not direct Harm reduction approaches, initiatives, programs, and services support
people on their journey towards positive change, as they define it.
Support is based on what PWUD identify as their needs and goals (not
what programs think they need), offering people tools to thrive.
Promote safety Harm reduction approaches, initiatives, programs, and services actively
promote safety as defined by the people they serve. These efforts
also acknowledge the impact that law enforcement can have on
PWUD (particularly in historically criminalized and marginalized
communities) and provide services accordingly.
Engage first Each community has different cultural strengths, resources,
challenges, and needs. Harm reduction approaches, initiatives,
programs, and services are grounded in the most impacted
and marginalized communities. It is important that meaningful
engagement and shared decision making begins in the design phase
of programming. Equally important is bringing to the table as many
individuals and organizations as possible who understand harm
reduction and who have meaningful relationships with the affected
communities.
Prioritize
listening
Each community has its own unique story that can be the foundation
for harm reduction work. When we listen deeply, we learn what
matters. Harm reductionists engage in active listening ― the act of
inviting people to express themselves completely, recognizing the
listener’s inherent biases, with the intent to fully absorb and process
what the speaker is saying.
Work toward
systems change
Harm reduction approaches, initiatives, programs, and services
recognize that trauma; social determinants of health, such as access
to healthcare, housing, and employment; inequitable policies; lack of
prevention and early intervention strategies; and social support have
all had a responsibility in systemic harm.
Harm Reducon Framework
12
Core Practice Areas
Core practices are effective methods for harm reduction that reflect community
understanding, experience, strengths, and needs. There are six core practice areas: (1)
safer practices; (2) safer settings; (3) safer access to healthcare; (4) safer transitions to care; (5)
sustainable workforce and field; and (6) sustainable infrastructure.
While not an exhaustive list, Table 3 provides key strategies and links to resources.
Anyone in the United States can access free, direct technical assistance (in any of the
core practice areas) from SAMHSA and CDC. SAMHSA’s harm reduction webpage offers
resources, including allowable expenses for its grants that support harm reduction activities.
Table 3. Core Practice Areas
Examples of Practices
Supporting Resources and Evidence
(Research- and Practice-based)
Safer Practices: Education and support describing how to reduce risk; provision of risk
reduction supplies and materials
Needs Based Syringe Services
Programs (SSPs) — also referred
to as syringe exchange programs
(SEPs) and needle exchange
programs (NEPs),* including
secondary exchange.
1,17,19,22,
26
,27,28,29
CDC Syringe Services Programs Technical Package
SAMHSA TIP 33 Treatment for Stimulant Use Disorders
SAMHSA TIP 63 Medications for Opioid Use Disorder
Safer smoking supplies/
distribution to reduce infectious
disease transmission.*
29,30,31
*As permitted by law. No
federal funding is used directly
or through subsequent
reimbursement of grantees to
purchase pipes. Grants include
explicit prohibitions of federal
funds to be used to purchase
drug paraphernalia.
CDC Stimulant Guide
Overdose education, overdose
detection services, and naloxone
distribution.
10,13,26,29,32
CDC Lifesaving Naloxone Guide
SAMHSA What is Naloxone?
SAMHSA TIP 63 Medications for Opioid Use Disorder
SAMHSA Opioid-Overdose Reduction Continuum of
Care Approach (ORCCA) Practice Guide 2023
Engaging Community Coalitions to Decrease Opioid
Overdose Deaths Practice Guide 2023
Harm Reducon Framework
13
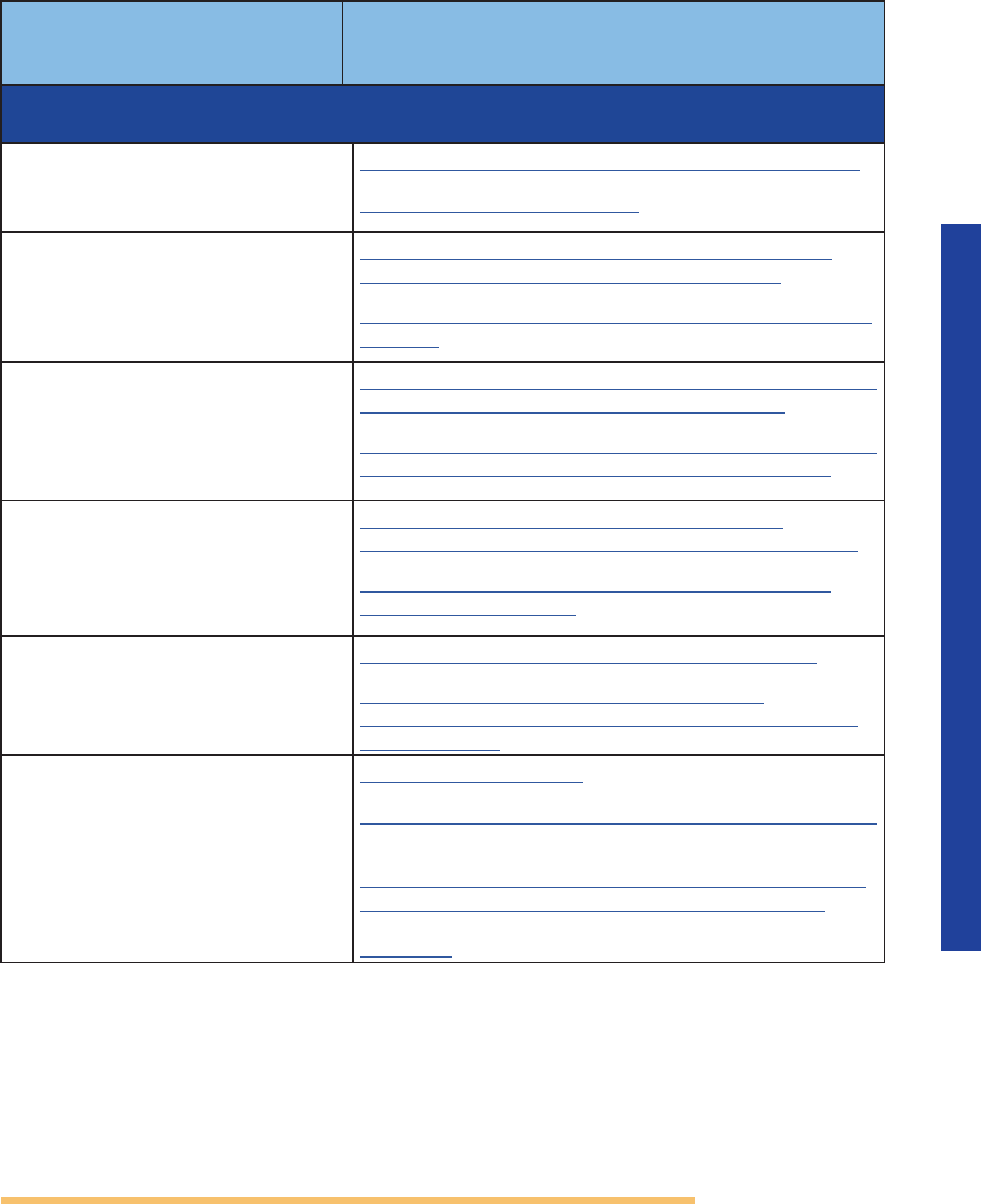
Examples of Practices
Supporting Resources and Evidence
(Research- and Practice-based)...(Cont.)
Drug-checking education,
fentanyl test strips, xylazine
test strips
and other assay test
strips, FTIR spectrometers, and
other drug-checking technology
at community drug-checking
sites.
33,34
CDC MMWR: Rapid Analysis of Drugs: A Pilot
Surveillance System to Detect Changes in the Illicit
Drug Supply to Guide Timely Harm Reduction
Responses
Overdose Data to Action: Surveillance Strategies |
Drug Overdose | CDC Injury Center
SAMHSA Federal Grantees May Now Use Funds to
Purchase Fentanyl Test Strips
Integrated reproductive health
education, services and supplies,
and sexually transmitted infection
screening, prevention, and
treatment.
35,36,37,38
SAMHSA TIP 33 Treatment for Stimulant Use Disorders
Onsite access or immediate
accessible referral to basic wound
care supplies and services in the
community.
38
Wound Care & Medical Triage for People Who Use
Drugs and the Programs That Serve Them | NASTAD
CDC Syringe Services Program Technical Package
Safer Settings: Access to safe environments to live, find respite, practice safer use, and
receive supports that are trauma-informed and stigma-free
Day centers and social spaces
that offer harm reduction
services, are low barrier, and
are led and maintained by the
communities they serve.
39
SAMHSA Peer Support Services in Crisis Care
Access to safe and secure
housing.
33,40
SAMHSA Homeless & Housing Resource Center
Public health programs as
alternatives to arrest and any legal
system involvement.
20,41
SAMHSA Criminal and Juvenile Justice Resources
Hybrid recovery community
organizations providing peer-
delivered harm reduction and
recovery support services.
42
Peer Recovery Center of Excellence
Harm Reducon Framework
14
Examples of Practices
Supporting Resources and Evidence
(Research- and Practice-based)...(Cont.)
Safer Access to Healthcare: Ensuring access to person-centered and non-stigmatizing
healthcare that is trauma informed, including FDA-approved medications
Low-barrier treatment services
that offer a whole-person
approach and rapid re-initiation,
if needed.
43
SAMHSA Practical Tools for Prescribing and Promoting
Buprenorphine in Primary Care Settings
Flexible provision of services
that offer medication starts at
first visit or at home, choice of
medications, and individualized
dosages.
44
SAMHSA Practical Tools for Prescribing and Promoting
Buprenorphine in Primary Care Settings
Healthcare settings and providers
are directly informed by harm
reduction principles, pillars, and
the people they serve.
45,46,47
SAMHSA Engaging Community Coalitions to Decrease
Opioid Overdose Deaths Practice Guide 2023
Nonpunitive care that
consistently offers the standard
of care in a nonstigmatizing,
nonjudgmental manner and
does not refuse healthcare based
on stigma or personal beliefs
about PWUD.
48
Overcoming Stigma, Ending Discrimination
Mobile access and take-home
methadone medication.
49,50,51,52
SAMHSA Methadone Take-Home Flexibilities
Extension Guidance
Mobile buprenorphine services,
including telehealth options
for initiation and continuity of
care.
53,54,55,56
SAMHSA The Physical Evaluation of Patients Who Will
Be Treated with Buprenorphine at Opioid Treatment
Programs
Access to new paradigms of care,
including treatment specific to
the use of all drugs and/or each
drug.
57,58
SAMHSA Treating Concurrent Substance Use Among
Adults
Onsite or quick referral
,
low-
barrier oral health services that
are informed by lived experience
of substance use
.
59
Oral Health, Mental Health and Substance Use
Treatment
Harm Reducon Framework
15
Examples of Practices
Supporting Resources and Evidence
(Research- and Practice-based)...(Cont.)
Safer Transitions to Care: Connections and access to harm-reduction-informed and
trauma-informed care and services
Health hubs for PWUD/ integrated
HIV, viral hepatitis, and healthcare
services.
26,38,60,61,62,63,64
Center of Excellence for Integrated Health Solutions
CDC HIV Risk Reduction Tool
Expand telehealth, while also
addressing low technology
literacy and enhancing access in
languages other than English.
54
SAMHSA Telehealth for the Treatment of Serious
Mental Illness and Substance Use Disorders
SAMHSA Culturally Competent LEP and Low-literacy
Services
Warm hand-off to and from
emergency department programs
― with low-barrier MOUD
initiation and post- overdose
services.
38,65
SAMHSA Connecting Communities to Substance Use
Services: Practical Tools for First Responders
ACA Expanding Access to Medications for Opioid Use
Disorder in Corrections and Community Settings
Medication access and treatment
on-demand (abstinence not
required).
26,66,67,68
SAMHSA Practical Tools for Prescribing and
Promoting Buprenorphine in Primary Care Settings
CDC Linking People with Opioid Use Disorder to
Medication Treatment
Onsite or immediate referral to
accessible nutritional assistance,
clothing, temporary shelter, and
housing.
65
SAMHSA Homeless & Housing Resource Center
SAMHSA Expanding Access to and Use of
Behavioral Health Services for People Experiencing
Homelessness
Seamless coordination of care
for individuals leaving carceral
settings and treatment settings
that do not offer medications,
because people are at greatly
heightened risk for overdose
fatality when back in the
community.
65
SAMHSA GAINS Center
ACA Expanding Access to Medications for Opioid Use
Disorder in Corrections and Community Settings
SAMHSA Best Practices for Successful Reentry from
Criminal Justice Settings for People Living With
Mental Health Conditions and/or Substance Use
Disorders
Harm Reducon Framework
16
Examples of Practices
Supporting Resources and Evidence
(Research- and Practice-based)...(Cont.)
Sustainable Workforce and Field: Resources for maintaining a skilled, well-supported,
and appropriately managed workforce and for sustaining community-based programs
Organizational leadership from
people with living and lived
experience.
26
ASPE Methods and Emerging Strategies to Engage
People with Lived Experience
SAMHSA Participation Guidelines for Individuals with
Lived Experience and Family
NHRC Peer Delivered Syringe Exchange (PDSE)
Toolkit
SAMHSA TIP 64: Incorporating Peer Support into
Substance Use Disorder Treatment Services
Living wages and essential
benefits for harm reduction
workers.
69,70
SAMHSA National Model Standards for Peer Support
Certification
Wellness services and support
for harm reduction staff and
volunteers without mandated
abstinence.
39,71
SAMHSA National Model Standards for Peer Support
Certification
Training and technical assistance
for community-based providers.
38
SAMHSA Practitioner Training
Include harm reduction expertise
and lived expertise in the selection
process of reviewers for harm
reduction grants and other
competitive processes.
72
SAMHSA Grant Review Process
Sustainable Infrastructure:
Resources for building and maintaining a revitalized
and community-led infrastructure to support harm reduction best practices and
the needs of PWUD
Hire and appropriately compensate
PWUD to inform policy at agencies
that serve PWUD.
73
SAMHSA National Model Standards for Peer Support
Certification
Co-leadership of PWUD in
organizational partnership in
research.
74
SAMHSA National Model Standards for Peer Support
Certification
Promote education on the value of
harm reduction services.
26,75, 76,77,78,79
CDC/SAMHSA National Harm Reduction Technical
Assistance Center
SAMHSA Harm Reduction
SAMHSA National Model Standards for Peer Support
Certification

Harm Reducon Framework
17
Community-Based Harm Reduction Programs (CHRPs)
While integrating harm reduction (as an approach and as services) into a wide variety
of settings is beneficial to the people who are served and impacted by them, SAMHSA
is committed to supporting harm reduction organizations that are by and for their
community ― as they are mission critical for connecting to our communities’ most
marginalized individuals.
CHRPs describe harm reduction organizations where people with lived and living
experience lead the planning and oversight, program development and evaluation, and
resource/funding allocation for an organization’s harm reduction initiatives, programs, and
services. CHRPs also offer the core practice areas, as permitted by law. Harm reduction
activities may be integrated into a comprehensive, person-centered program of care that
includes treatment services that meet the specific needs of the community in which the
program is housed.
In addition to programs being consistent with
all aforementioned principles and pillars,
CHRPs should include people with lived experience as co-investigators in any research
project. Boards, staff, and team members should be at least 51 percent those with lived
experience. CHRPs demonstrate meaningful connection to PWUD in their community,
especially to communities most marginalized, and provide lowest-barrier, core harm
reduction practices.
Conclusion
The Harm Reduction Summit was a groundbreaking event that engaged a diversity of
perspectives across the fields of prevention, treatment, recovery, and harm reduction. More
than 100 participants attended the Summit, representing the private sector, community-
based organizations, health care, faith-based organizations, academia, researchers, funders,
law enforcement, and leaders from federal, state, local, and tribal governments.
The subsequent Steering Committee synthesized and refined the Summit findings,
providing guidance for this Framework. Moving forward, this Framework will inform
SAMHSA’s harm reduction activities, as well as related policies, programs, and practices.
SAMHSA’s aim is to integrate harm reduction activities and approaches across its
organizational Centers and initiatives, and to do so in a manner that draws on evidence-
based practice and principles — while also maintaining sustained dialog with harm
reductionists and PWUD.
SAMHSA is committed to continued collaboration with PWUD and the field to put this
Framework into practice, support and expand harm reduction approaches and services,
and ultimately save lives.

Harm Reducon Framework
18
References
1
Abdul-Quader, A.S., Feelemyer, J., Modi, S., & Des Jarlais, D.C. (2013). Effectiveness of structural-
level needle/syringe programs to reduce HCV and HIV infection among people who inject
drugs: a systematic review. AIDS Behavior, 17, 2878–2892. https://doi.org/10.1007/s10461-013-
0593-y
2
Office of National Drug Control Policy. (2022). National Drug Control Strategy. https://www.
whitehouse.gov/ondcp/the-administrations-strategy/national-drug-control-strategy/
3
Hagan, H., McGough, J.P., Thiede, H., Hopkins, S., Duchin, J., & Alexander, E.R. (2000). Reduced
injection frequency and increased entry and retention in drug treatment associated with
needle exchange participation in Seattle drug injectors. Journal of Substance Abuse
Treatment, 19(3), 247-252. https://doi.org/10.1016/S0740-5472(00)00104-5
4
Haffajee, R.L., Sherry, T.B., Dubenitz, J.M., White, J.O., Schwartz, D., Stoller, B., & Bagalman, E.
(2021). U.S. Department of Health and Human Services Overdose Prevention Strategy (Issue
Brief). U.S. Department of Health and Human Services. https://aspe.hhs.gov/sites/default/files/
documents/101936da95b69acb8446a4bad9179cc0/overdose-prevention-strategy.pdf
5
Des Jarlais, D.C. (2017). Harm reduction in the USA: the research perspective and an archive to
David Purchase. Harm Reduction Journal, 14, Article 51. https://doi.org/10.1186/s12954-017-0178-6
6
Centers for Disease Control. (1982). Acquired immune deficiency syndrome (AIDS): precautions
for clinical and laboratory staffs. MMWR, 31(43), 577–580. https://www.cdc.gov/mmwr/preview/
mmwrhtml/00001183.htm
7
McLean K. (2011). The biopolitics of needle exchange in the United States. Critical Public
Health, 21(1), 71–79. https://doi.org/10.1080/09581591003653124
8
The Public Health and Welfare Act, 42 U.S.C. § 300ee-5. (2009). Use of funds to supply
hypodermic needles or syringes for illegal drug use; prohibition. https://www.govinfo.gov/
content/pkg/USCODE-2009-title42/pdf/USCODE-2009-title42-chap6A-subchapXXIII-partA-
sec300ee-11.pdf
9
National Harm Reduction Coalition. (2021). Who we are. https://harmreduction.org/about-us/
10
Wheeler, E., Jones, T.S., Gilbert, M.K., Davidson, P.J., & Centers for Disease Control and
Prevention (CDC). (2015). Opioid overdose prevention programs providing naloxone to
laypersons—United States, 2014. MMWR, 64(23), 631–635. https://www.cdc.gov/mmwr/preview/
mmwrhtml/mm6423a2.htm
11
Ibid.
12
Ibid.
13
Lambdin, B.H., Bluthenthal, R.N., Wenger, L.D., Wheeler, E., Garner, B., Lakosky, P., & Kral, A.H.
(2020). Overdose education and naloxone distribution within syringe service programs—
United States, 2019. MMWR, 69(33), 1117–1121. https://www.cdc.gov/mmwr/volumes/69/wr/
mm6933a2.htm
14
Mueller, S.R., Walley, A.Y., Calcaterra, S.L., Glanz, J.M., & Binswanger, I.A. (2015). A review of
opioid overdose prevention and naloxone prescribing: implications for translating community
programming into clinical practice. Substance Abuse, 36(2), 240–253. https://doi.org/10.1080/08
897077.2015.1010032

Harm Reducon Framework
19
15
Aspinall, E.J., Nambiar, D., Goldberg, D.J., Hickman, M., Weir, A., Van Velzen, E., & Hutchinson,
S.J. (2014). Are needle and syringe programmes associated with a reduction in HIV
transmission among people who inject drugs: a systematic review and meta-analysis.
International Journal Epidemiology, 43(1), 235–248. https://pubmed.ncbi.nlm.nih.gov/24374889/
16
van Santen, D.K., Lodi, S., Dietze, P., van den Boom, W., Hayashi, K., Dong, H., & Prins, M.
(2023). Comprehensive needle and syringe program and opioid agonist therapy reduce
HIV and hepatitis C virus acquisition among people who inject drugs in different settings: a
pooled analysis of emulated trials. Addiction, 118(6), 1116–1126. https://pubmed.ncbi.nlm.nih.
gov/36710474/
17
Centers for Disease Control and Prevention. (2019). Summary of Information on the safety and
effectiveness of Syringe Services Programs (SSPs). https://www.cdc.gov/ssp/syringe-services-
programs-summary.html
18
Executive Order No. 13985, 86 Fed. Reg. 7009 (January 20, 2021). Advancing racial equity and
support for underserved communities through the federal government. Federal Register.
https://www.federalregister.gov/documents/2021/01/25/2021-01753/advancing-racial-equity-
and-support-for-underserved-communities-through-the-federal-government
19
Substance Abuse and Mental Health Services Administration (SAMHSA). (2022). Community
engagement: an essential component of an effective and equitable substance use
prevention system. SAMHSA. https://store.samhsa.gov/product/community-engagement-
essential-component-substance-use-prevention-system/pep22-06-01-005
20
Substance Abuse and Mental Health Services Administration (SAMHSA). (2022). Behavioral
health equity. SAMHSA. https://www.samhsa.gov/behavioral-health-equity
21
Substance Abuse and Mental Health Services Administration (SAMHSA). (2020). The opioid
crisis and the Black/African American population: an urgent issue. SAMHSA. https://store.
samhsa.gov/product/The-Opioid-Crisis-and-the-Black-African-American-Population-An-
Urgent-Issue/PEP20-05-02-001
22
Zulqarnain, J., Burk, K., Facente, S., Pegram, L., Ali, A., & Asher, A. (2020). Syringe services
program: a technical package of effective strategies and approaches for planning, design,
and implementation. Centers for Disease Control and Prevention. https://stacks.cdc.gov/view/
cdc/105304
23
Ditmore, M.H. (2013). When sex work and drug use overlap: considerations for advocacy and
practice. Harm Reduction International. https://www.hri.global/files/2014/08/06/Sex_ work_
report_%C6%924_WEB.pdf
24
Substance Abuse and Mental Health Services Administration (SAMHSA). (2010). Shared decision-
making in mental health care: practice, research, and future directions. SAMHSA. https://store.
samhsa.gov/product/Shared-Decision-Making-in-Mental-Health-Care/SMA09-4371
25
Ti, L., Tzemis, D., & Buxton, J.A. (2012). Engaging people who use drugs in policy and program
development: A review of the literature. Substance Abuse Treatment, Prevention, and Policy,
7(1), 47–47. https://doi.org/10.1186/1747-597X-7-47
26
Broz, D., Carnes, N., Chapin-Bardales, J., Des Jarlais, D.C., Jones, C.M., McClung, R.P., & Asher,
A.K. (2021). Syringe services programs’ role in ending the HIV epidemic in the U.S.: why we
cannot do it without them. American Journal of Preventive Medicine, 61(5, Suppl. 1), S118-S129.
https://doi.org/10.1016/j.amepre.2021.05.044

Harm Reducon Framework
20
27
National Institute on Drug Abuse. (2022). Syringe services programs. https://nida.nih.gov/drug-
topics/syringe-services-programs
28
Centers for Disease Control and Prevention. (2021). HIV prevention in the United States:
mobilizing to end the epidemic. https://stacks.cdc.gov/view/cdc/103438
29
Kral, A.H., Lambdin, B.H., Browne, E.N., Wenger, L.D., Bluthenthal, R.N., Zibbell, J.E., & Davidson,
P.J. (2021). Transition from injecting opioids to smoking fentanyl in San Francisco, California.
Drug and Alcohol Dependence, 227, 109003. https://pubmed.ncbi.nlm.nih.gov/34482046
30
Strike, C., & Watson, T.M. (2017). Education and equipment for people who smoke
crack cocaine in Canada: progress and limits. Harm Reduction Journal, 14(17). https://
harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-017-0144-3
31
Centers for Disease Control and Prevention (CDC). (2023). CDC Stimulant Guide. CDC. https://
www.cdc.gov/drugoverdose/featured-topics/stimulant-guide.html#q10
32
Weiner, J., Murphy, S.M., & Behrends, C. (2019). Expanding access to naloxone: a review of
distribution strategies. Leonard Davis Institute of Health Economics, Center for Health
Economics of Treatment Interventions for Substance Use Disorder, HCV, and HIV. https://
ldi.upenn.edu/our-work/research-updates/expanding-access-to-naloxone-a-review-of-
distribution-strategies/
33
Park, J.N., Frankel, S., Morris, M., Dieni, O., Fahey-Morrison, L., Luta, M., & Sherman, S. (2021).
Evaluation of fentanyl test strip distribution in two Mid-Atlantic syringe services programs.
International Journal of Drug Policy, 94, 103196. https://pubmed.ncbi.nlm.nih.gov/33713964
34
Peiper, N.C., Clarke, S.D., Vincent, L., Ciccarone, D., Kral, A.H., & Zibbell, J.E. (2019). Fentanyl test
strips as an opioid overdose prevention strategy: Findings from a syringe services program
in the Southeastern United States. International Journal of Drug Policy, 63, 122–128. https://
pubmed.ncbi.nlm.nih.gov/30292493
35
Owens, L., Gilmore, K., Terplan, M., Prager, S., & Micks, S. (2020). Providing reproductive health
services for women who inject drugs: a pilot program. Harm Reduction Journal, 17(47). https://
harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-020-00395-y
36
Burr, C.K., Storm, D.S., Hoyt, M.J., Dutton, L., Berezny, L., Allread, V., & Paul, S. (2014). Integrating
health and prevention services in syringe access programs: a strategy to address unmet
needs in a high-risk population. Public Health Reports, 129(1), 26–32. https://www.ncbi.nlm.nih.
gov/pmc/articles/PMC3862985
37
Centers for Disease Control and Prevention. (2022). HIV risk among persons who exchange sex
for money or nonmonetary items. https://www.cdc.gov/hiv/group/sexworkers.html
38
Centers for Disease Control and Prevention. (2016). Program guidance for implementing
certain components of syringe services programs. https://www.cdc.gov/hiv/pdf/risk/cdc-hiv-
syringe-exchange-services.pdf
39
Olding, M., Ivsins, A., Mayer, S., Betsos, A., Boyd, J., Sutherland, C., & McNeil, R. (2020). A low-
barrier and comprehensive community-based harm-reduction site in Vancouver, Canada.
American Journal of Public Health, 110(6), 833–835. https://pubmed.ncbi.nlm.nih.gov/32298171/

Harm Reducon Framework
21
40
Watson, D.P., Shuman, V., Kowalsky, J., Golembiewski, E., & Brown, M. (2017). Housing first and
harm reduction: a rapid review and document analysis of the US and Canadian open access
literature. Harm Reduction Journal, 14(30). https://harmreductionjournal.biomedcentral.com/
articles/10.1186/s12954-017-0158-x
41
Volkow, N.D., Poznyak, V., Saxena, S., Gerra, G., & UNODC-WHO Informal International Scientific
Network (2017). Drug use disorders: impact of a public health rather than a criminal justice
approach. World Psychiatry, 16(2), 213–214. https://doi.org/10.1002/wps.20428
42
Ashford, R.D., Brown, A.M., McDaniel, J., Neasbitt, J., Sobora, C., Riley, R., & Curtis, B. (2019).
Responding to the opioid and overdose crisis with innovative services: the Recovery
Community Center Office-Based Opioid Treatment (RCC-OBOT) model. Addictive Behaviors,
98, 106031. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7286074/
43
Aronowitz, S.V., Navos Behrends, C., Lowenstein, M., Schackman, B.R., & Weiner, J. (2022).
Lowering the barriers to medication treatment for people with opioid use disorder. Leonard
Davis Institute of Health Economics, Center for Health Economics of Treatment Interventions
for Substance Use Disorder, HCV, and HIV. https://ldi.upenn.edu/wp-content/uploads/2022/01/
Penn-LDI.CHERISH-Issue-Brief.January-2022.pdf
44
Jakubowski A., & Fox A. (2020). Defining low-threshold buprenorphine treatment. Journal of
Addiction Medicine, 14(2), 95–98. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7075734/
45
Hawk, M., Coulter, R.W., Egan, J.E., Fisk, S., Reuel Friedman, M., Tula, M., & Kinsky, S. (2017).
Harm reduction principles for healthcare settings. Harm Reduction Journal, 14, Article 70.
https://harmreductionjournal.biomedcentral.com/articles/10.1186/s12954-017-0196-4
46
Khan, G.K., Harvey, L., Johnson, S., Long, P., Kimmel, S., Pierre, C., & Drainoni, M.-L. (2022).
Integration of a community-based harm reduction program into a Safety Net Hospital:
A qualitative study. Harm Reduction Journal, 19, Article 35. https://harmreductionjournal.
biomedcentral.com/articles/10.1186/s12954-022-00622-8
47
Krawczyk, N., Allen, S.T., Schneider, K.E., Solomon, K., Shah, H., Morris, M., & Saloner, B.
(2022). Intersecting substance use treatment and harm reduction services: exploring the
characteristics and service needs of a community-based sample of people who use drugs.
Harm Reduction Journal, 19, Article 95. https://pubmed.ncbi.nlm.nih.gov/36002850/
48
Muncan, B., Walters, S.M., Ezell, J., & Ompad, D.C. (2020). “They look at us like junkies”:
Influences of drug use stigma on the healthcare engagement of people who inject drugs
in New York City. Harm Reduction Journal, 17, Article 53. https://doi.org/10.1186/s12954-020-
00399-8
49
Chan, B., Hoffman, K.A., Bougatsos, C., Grusing, S., & Chou, R. (2021). Mobile methadone
medication units: A brief history, scoping review and research opportunity. Journal of
Substance Abuse Treatment, 129, Article 108483. https://pubmed.ncbi.nlm.nih.gov/34080541/
50
Greenfield, L., Brady, J.V., Besteman, K.J., & De Smet, A. (1996). Patient retention in mobile and
fixed-site methadone maintenance treatment. Alcohol and Drug Dependence, 42, 125–131.
https://pubmed.ncbi.nlm.nih.gov/8889411/
51
Frank, D. Mateu-Gelabert, P., Perlman, D.C., Walters, S.M., Curran, L., & Guarino, H. (2021). “It’s
like ‘liquid handcuffs’”: The effect of take-home dosing policies on methadone maintenance
treatment (MMT) patients’ lives. Harm Reduction Journal, 18, Article 88. https://doi.org/10.1186/
s12954-021-00535-y

Harm Reducon Framework
22
52
Amram, O., Amiri, S., Panwala, V., Lutz, R., Joudrey, P.J. & Socias, E. (2021). The impact of
relaxation of methadone take-home protocols on treatment outcomes in the COVID-19 era.
American Journal of Drug and Alcohol Abuse, 47(6), 722–729. https://www.tandfonline.com/
doi/abs/10.1080/00952990.2021.1979991?journalCode=iada20
53
Rosecrans, A., Harris, R., Saxton, R.E., Cotterell, M., Zoltick, M., Willman, C., & Page, K.R. (2022).
Mobile low- threshold buprenorphine integrated with infectious disease services. Journal of
Substance Abuse Treatment, 133, Article 108553. https://doi.org/10.1016/j.jsat.2021.108553
54
Inheanacho, T., Payne, K., & Tsai, J. (2020). Mobile, community-based buprenorphine treatment
for veterans experiencing homelessness with opioid use disorder: a pilot, feasibility study.
American Journal of Addiction, 29(6), 485–491. https://pubmed.ncbi.nlm.nih.gov/32367557/
55
Krawczyk, N., Buresh, M., Gordon, M.S., Blue, T.R., Fingerhood, M.I., & Agus, D. (2019). Expanding
low-threshold buprenorphine to justice-involved individuals through mobile treatment:
Addressing a critical care gap. Journal of Substance Abuse Treatment, 103, 1–8. https://
pubmed.ncbi.nlm.nih.gov/31229187
56
Gibson, B.A., Morano, J.P., Walton, M.R., Marcus, R., Zelenev, A., Bruce, R.D., & Altice, F.L. (2017).
Innovative program delivery and determinants of frequent visitation to a mobile medical
clinic in an urban setting. Journal of Health Care for the Poor and Underserved, 28(2), 643–
662. https://pubmed.ncbi.nlm.nih.gov/28529215
57.
Robbins, J.L., Englander, H., & Gregg, J. (2021). Buprenorphine microdose induction for the
management of prescription opioid dependence. Journal of the American Board of Family
Medicine, 34, S141–S146. https://pubmed.ncbi.nlm.nih.gov/33622829/
58
Randhawa, P.A., Brar, R., & Nolan, S. (2020). Buprenorphine-naloxone “microdosing”: an
alternative induction approach for the treatment of opioid use disorder in the wake of North
America’s increasingly potent illicit drug market. Canadian Medical Association Journal,
192(3). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6970598/#:~:text=Officially%20
recognized%20as%20the%20Bernese,over%20time%20(Box%201).
59
National Council for Mental Wellbeing. (2021). Oral health, mental health and substance
use treatment. https://www.thenationalcouncil.org/wp-content/uploads/2021/09/NC_CoE_
OralhealthMentalHealthSubstanceUseChallenges_Toolkit.pdf?daf=375ateTbd56&sc_cid=SG_
Refer_blog_mouth-body-connection_link-between-mental-health-and-oral-health
60
Palmateer, N., Hamill, V., Bergenstrom, A., Bloomfield, H., Gordon, L., Stone, & Hutchinson, S.
(2022). Interventions to prevent HIV and hepatitis C among people who inject drugs: latest
evidence of effectiveness from a systematic review (2011 to 2020). International Journal of
Drug Policy, 109, Article 103872. https://doi.org/10.1016/j.drugpo.2022.103872
61
Rich, K.M., Bia, J., Altice, F.L. et al. (2018). Integrated models of care for individuals with opioid
use disorder: how do we prevent HIV and HCV?. Current HIV/AIDS Reports, 15, 266–275. https://
doi.org/10.1007/s11904-018-0396-x
62
Mette, E. (2020). Q&A: A deep dive into New York’s Drug User Health Hubs with New York’s
Allan Clear. National Academy for State Health Policy. https://www.nashp.org/qa-a-deep-dive-
into-new-yorks-drug-user-health-hubs-with-new-yorks-allan-clear/

Harm Reducon Framework
23
63
Eckhardt, B., Mateu-Gelabert, P., Aponte-Melendez, Y., Fong, C., Kapadia, S., Smith, M.,
Edlin, B. R., & Marks, K.M. (2022). Accessible hepatitis C care for people who inject drugs: a
randomized clinical trial. JAMA Internal Medicine, 182(5), 494–502. https://jamanetwork.com/
journals/jamainternalmedicine/fullarticle/2790054
64
Bartholomew, T.S., Tookes, H.E., Serota, D.P., Behrends, C.N., Forrest, D.W., & Feaster, D.J.
(2020). Impact of routine opt-out HIV/HCV screening on testing uptake at a syringe services
program: an interrupted time series analysis. International Journal of Drug Policy, 84, Article
102875. https://pubmed.ncbi.nlm.nih.gov/32731112
65
Substance Abuse and Mental Health Services Administration (SAMHSA). (2022). Harm
Reduction. SAMHSA. https://www.samhsa.gov/find-help/harm-reduction
66
Platt, L., Minozzi, S., Reed, J., Vickerman, P., Hagan, H., French, C., & Hickman, M. (2017). Needle
syringe programmes and opioid substitution therapy for preventing hepatitis C transmission
in people who inject drugs. Cochrane Database of Systematic Reviews, 9, CD012021. https://
pubmed.ncbi.nlm.nih.gov/28922449/
67
Weinstein, Z.M., Cheng, D.M., D’Amico, M.J., Forman, L.S., Regan, D., Yurkovic, A., Samet,
J.H., & Walley, A.Y. (2020). Inpatient addiction consultation and post-discharge 30-day
acute care utilization. Drug and Alcohol Dependence, 213, 108081. https://doi.org/10.1016/j.
drugalcdep.2020.108081
68
Payne, B.E., Klein, J.W., Simon, C.B., James, J.R., Jackson, S.L., Merrill, J.O., Zhuang, R., & Tsui,
J.I. (2019). Effect of lowering initiation thresholds in a primary care-based buprenorphine
treatment program. Drug and Alcohol Dependence, 200, 71–77. https://pubmed.ncbi.nlm.nih.
gov/31103879/
69
Olding, M., Barker, A., McNeil, R., & Boyd, J. (2021). Essential work, precarious labour: the need
for safer and equitable harm reduction work in the era of COVID-19. International Journal of
Drug Policy, 90, Article 103076. https://pubmed.ncbi.nlm.nih.gov/33321286/
70
Greer, A., Bungay, V., Pauly, B., & Buxton, J. (2020). ‘Peer’ work as precarious: A qualitative study
of work conditions and experiences of people who use drugs engaged in harm reduction
work. International Journal of Drug Policy, 85, Article 102922. https://pubmed.ncbi.nlm.nih.
gov/32911320/
71
Shepard, B.C. (2013). Between harm reduction, loss and wellness: on the occupational hazards
of work. Harm Reduction Journal, 10(5). https://harmreductionjournal.biomedcentral.com/
articles/10.1186/1477-7517-10-5
72
Rittenbach, K., Horne, C.G., O’Riordan, T., Bichel, A., Mitchell, N., Fernandez Parra, A.M., &
MacMaster, F.P. (2019). Engaging people with lived experience in the grant review process.
BMC Medical Ethics, 20, Article 95. https://doi.org/10.1186/s12910-019-0436-0
73
Marshall, Z., Dechman, M.K., Minichiello, A., Alcock, L., & Harris, G.E. (2015). Peering into the
literature: A systematic review of the roles of people who inject drugs in harm
reduction initiatives. Drug and Alcohol Dependence, 151, 1–14. https://pubmed.ncbi.nlm.nih.
gov/25891234/
74
Brown, G., Crawford, S., Perry, G.E., Byrne, J., Dunne, J., Reeders, D., & Jones, S. (2019). Achieving
meaningful participation of people who use drugs and their peer organizations in a strategic
research partnership. Harm Reduction Journal, 16(1), 37. https://harmreductionjournal.
biomedcentral.com/articles/10.1186/s12954-019-0306-6

Harm Reducon Framework
24
75
Fernandez-Vina, M.H., Prood, N.E., Herpolsheimer, A., Waimber, J., & Burris, S. (2020). State laws
governing syringe services programs and participant syringe possession, 2014–2019. Public
Health Reports, 135(S1), 128S–137S. https://pubmed.ncbi.nlm.nih.gov/32735195/
76
Davis, C.S., Burris, S., Kraut-Becher, J., Lynch, K.G., & Metzger, D. (2005). Effects of an intensive
street-level police intervention on syringe exchange program use in Philadelphia, Pa.
American Journal of Public Health, 95(2), 233–236. https://www.ncbi.nlm.nih.gov/pmc/articles/
PMC1449157/
77
Jones, C.M. (2019). Syringe services programs: An examination of legal, policy, and funding
barriers in the midst of the evolving opioid crisis in the U.S. International Journal of Drug
Policy, 70, 22–32. https://pubmed.ncbi.nlm.nih.gov/31059965/
78
Cloud, D.H., Castillo, T., Brinkley-Rubinstein, L., Dubey, M., & Childs, R. (2018). Syringe
decriminalization advocacy in red states: lessons from the North Carolina Harm Reduction
Coalition. Current HIV/AIDS Reports, 15(3), 276–282. https://doi.org/10.1007/s11904-018-0397-9
79
Clark, P.A. & Fadus, M. (2010). Federal funding for needle exchange programs. Medical Science
Monitor, 16(1). https://pubmed.ncbi.nlm.nih.gov/20037499/

Harm Reducon Framework
25
Harm Reduction Steering
Committee Members
Mark Jenkins
Founder and Executive Director
Connecticut Harm Reduction Alliance
Hartford, CT
Elizabeth Burden
Senior Advisor
National Council for Mental Wellbeing
Phoenix, AZ
Jessica Tilley
Founder
HRH413
Northampton, MA
Hiawatha Collins
Community and Capacity Building Manager
National Harm Reduction Coalition
New York, NY
Sherrine Peyton
State Opioid Settlement Administrator
Illinois Department of Human Services
Chicago, IL
Rafael A. Torruella
Executive Director
Intercambios Puerto Rico
Fajardo, PR
Maya Doe-Simkins
Co-Founder
Harm Reduction Michigan
Traverse City, MI
Chad Sabora
Vice President of Government and Public
Relations
Indiana Center for Recovery
St. Louis, MO
Marielle A. Reataza
Executive Director
National Asian Pacific American Families
Against Substance Abuse
Alhambra, CA
Charles King
Chief Executive Officer
Housing Works
New York, NY
Justine Waldman
Founder and Chief Executive Officer
REACH Medical
Ithaca, NY
Rafael Rivera
Deputy Director
Bureau of Prevention Services, Illinois
Department of Human Services
Chicago, IL
Louise Vincent
Executive Director
North Carolina Urban Survivors Union
Greensboro, NC
Christine Rodriguez
Senior Program Manager
AIDS United
Washington, DC
Philomena Kebec
Economic Development Coordinator
Bad River Tribe
Odanah, WI
Caty Simon
Leadership Team Member
Urban Survivors Union
Holyoke, MA
Stephanie Campbell
Behavioral Ombudsman Project Director
New York State Office of Addiction Services
and Supports
Albany, NY
Anthony D. Salandy
Interim Executive Director, Managing Director
of Programs
National Harm Reduction Coalition
New York, NY
Chase Holleman
Public Health Analyst
Substance Abuse and Mental Health Services
Administration (SAMHSA)
Greensboro, NC
Shannon Mace
Executive Director
Legal Assistance Project: A Medical-Legal Partnership
Philadelphia, PA
[This page is intentionally blank.] [This page is intentionally blank.]
[This page is intentionally blank.] [This page is intentionally blank.]
Substance Abuse and Mental Health
Services Administration
SAMHSA’s mission is to lead public health and service delivery eorts that promote mental
health, prevent substance misuse, and provide treatments and supports to foster recovery while
ensuring equitable access and better outcomes.
1-877-SAMHSA-7 (726-4727) • 1-800-487-4889 (TTY) www.samhsa.gov
